
Can You Have an Ectopic Pregnancy with IVF?
April 13, 2025
Can You Pick the Gender with IVF?
April 13, 2025When Did IVF Begin? A Deep Dive into the History of In Vitro Fertilization
When Did IVF Begin? A Deep Dive into the History of In Vitro Fertilization
Imagine a world where starting a family feels out of reach for some. Now picture a groundbreaking solution that changes everything. That’s the story of in vitro fertilization, or IVF—a game-changer in reproductive medicine that’s helped millions of people become parents. But when did this incredible journey begin? Let’s travel back in time, uncover the roots of IVF, and explore how it evolved into the life-changing technology we know today.
IVF didn’t just pop up overnight. It’s a tale of curiosity, persistence, and a few brilliant minds who dared to push boundaries. From early experiments with rabbit eggs to the birth of the first “test-tube baby,” the history of IVF is full of surprises, setbacks, and triumphs. Along the way, we’ll dig into questions you might not find answered everywhere—like how scientists cracked the code of fertilization outside the body, what challenges they faced, and what’s next for this field. Ready? Let’s get started.
The Early Sparks: Where It All Began
The story of IVF starts long before the flashy labs and high-tech tools we picture today. It began in the late 19th century with a scientist named Samuel Leopold Schenk. In 1878, Schenk, a Viennese embryologist, was tinkering with rabbit and guinea pig eggs. He mixed them with sperm in a dish and watched something amazing happen—cell division. This wasn’t full-on IVF as we know it, but it was a spark. Schenk showed that life could start outside a living body, planting a seed for what would come decades later.
Fast forward to the 1930s, and another name enters the scene: Gregory Pincus. You might know him as one of the brains behind the birth control pill, but he was also a pioneer in reproductive science. In 1934, Pincus and his colleague Ernst Enzmann tried fertilizing rabbit eggs in a lab. They claimed success, but here’s the twist—later research suggests the fertilization might have happened inside the rabbit, not in the dish. Still, their work stirred up excitement and got people thinking: Could this work for humans?
Around the same time, scientists were figuring out the basics of how eggs and sperm work. In 1827, Karl Ernst von Baer had discovered the human egg, and by the 1940s, researchers like John Rock and Miriam Menkin were retrieving human eggs and trying to fertilize them. In 1944, Menkin made history by fertilizing a human egg in a lab dish—a huge step toward IVF. These early efforts were like puzzle pieces slowly coming together, setting the stage for the big breakthrough.
The Big Moment: The Birth of Louise Brown
Now, let’s jump to the moment that changed everything—July 25, 1978. On that day, in a small hospital in Oldham, England, a baby girl named Louise Brown was born. She wasn’t just any baby—she was the world’s first child conceived through IVF. Her parents, Lesley and John Brown, had struggled with infertility for years due to blocked fallopian tubes. Enter two brilliant minds: Dr. Patrick Steptoe, a gynecologist, and Robert Edwards, a physiologist.
Steptoe and Edwards teamed up in the late 1960s with a bold idea—fertilize an egg outside the body and place it back in the womb. It sounds simple now, but back then, it was revolutionary. They faced tons of hurdles, like figuring out how to retrieve eggs safely and keep embryos alive in a lab. Steptoe used a technique called laparoscopy—a fancy way of saying he made a tiny incision to grab eggs from Lesley’s ovaries. Edwards, meanwhile, perfected the lab conditions to make fertilization work.
After years of trial and error (and over 100 failed attempts), they hit the jackpot. Lesley’s egg was fertilized with John’s sperm in a petri dish, and the resulting embryo was transferred back into her uterus. Nine months later, Louise arrived via C-section, weighing 5 pounds, 12 ounces. The world went wild—some called it a miracle, others a controversy. Edwards even won a Nobel Prize in 2010 for his work (sadly, Steptoe had passed away by then). That day in 1978 wasn’t just a birth—it was the start of a new era.
Almost There: The Unsung Heroes Before 1978
Louise might have been the first IVF baby, but she wasn’t the only milestone. Just 67 days later, on October 3, 1978, a baby girl named Durga was born in India, conceived through IVF by Dr. Subhash Mukhopadhyay. Working with basic tools—like a household fridge to store samples—Mukhopadhyay pulled off an incredible feat. Sadly, his work wasn’t recognized at the time. Authorities blocked him from sharing it, and it took years for the world to give him credit. His story reminds us that IVF’s history isn’t just one path—it’s a web of efforts across the globe.
Back in the U.S., another near-miss happened in 1973. Dr. Landrum Shettles at Columbia University tried IVF, but his boss stopped him at the last second. Imagine how close they were! And in Australia, the Monash University team reported a short-lived IVF pregnancy in 1973—proof that others were hot on the trail. These “almosts” show how many people were racing toward the same goal, each adding a piece to the puzzle.
How Did They Figure It Out? The Science Behind IVF’s Start
So, how did scientists go from rabbit eggs to human babies? It’s all about cracking the code of fertilization. In the 1950s, two researchers—Min Chueh Chang in the U.S. and Colin Russell Austin in Australia—discovered something key: sperm needs to “mature” in the body before it can fertilize an egg. This process, called capacitation, was a game-changer. Chang proved it in 1959 by using IVF to birth a rabbit, showing the technique could work.
For humans, the challenge was bigger. Eggs are delicate, and the womb is picky. Edwards spent years tweaking lab conditions—think special fluids and precise timing—to mimic the body. Steptoe’s laparoscopy skills were clutch, too, letting him snag eggs without major surgery. By the 1970s, they’d nailed the recipe: retrieve eggs, fertilize them in a dish, grow the embryo for a few days, and transfer it back. It was a mix of biology, chemistry, and a little luck.
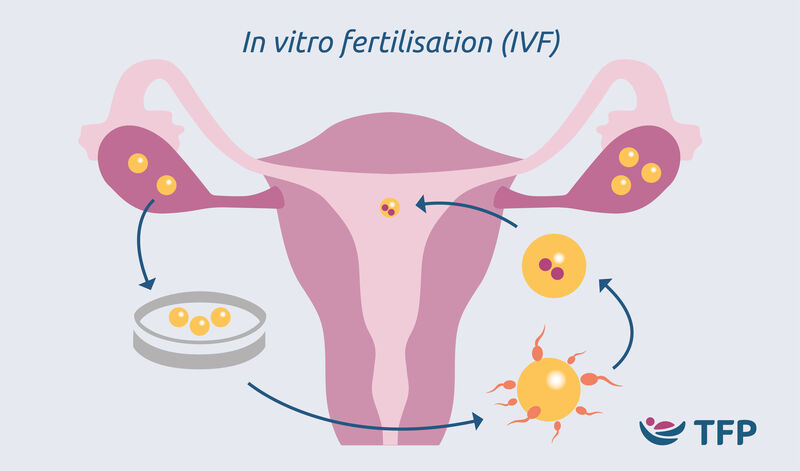
Here’s a quick breakdown of the early IVF process:
- Egg Retrieval: Using laparoscopy, doctors collected eggs from the ovaries.
- Fertilization: Sperm and egg met in a petri dish with a special nutrient mix.
- Embryo Growth: The fertilized egg grew for 2-3 days into an 8-cell embryo.
- Transfer: The embryo was placed in the uterus, hoping it would implant.
Simple, right? Not really—it took decades of failures to get there.
What Took So Long? Challenges and Controversies
IVF’s road to success was bumpy. For one, the science was tricky. Early attempts often failed because eggs wouldn’t fertilize or embryos wouldn’t survive. Labs back then weren’t fancy—think makeshift setups with basic microscopes. Plus, timing was everything; miss the egg’s “ripe” window, and it was game over.
Then there were the critics. Some called IVF unnatural or unethical, worrying about “designer babies” or playing God. Religious groups and governments got involved, slowing things down. In the U.S., funding for embryo research was (and still is) limited by laws like the Dickey-Wicker Amendment. Even Steptoe and Edwards faced pushback—people thought they were mad scientists. But they kept going, proving the doubters wrong one baby at a time.
IVF Goes Global: From One Baby to Millions
After Louise, IVF didn’t stay in England—it spread fast. In 1981, the first U.S. IVF baby, Elizabeth Carr, was born in Virginia. Australia followed with its own successes, thanks to teams like Monash. By the 1990s, IVF was popping up everywhere, from Japan to Brazil. Today, over 8 million babies have been born via IVF worldwide, according to estimates from 2018. That’s a lot of families!
What fueled this boom? Demand was one thing—about 1 in 7 couples struggle with infertility. Plus, technology got better. Freezing embryos (cryopreservation) became a thing in the 1980s, letting people save extras for later. A technique called ICSI (intracytoplasmic sperm injection), started in 1992, helped men with low sperm counts. Success rates jumped from a measly 6% in the early days to nearly 50% for women under 35 today.
A Fun Quiz: How Much Do You Know About IVF’s Beginnings?
Think you’ve got the basics down? Test yourself with this quick quiz:
- When was the first IVF baby born?
A) 1968 B) 1978 C) 1988 - Who were the two main scientists behind it?
A) Pincus and Chang B) Steptoe and Edwards C) Rock and Menkin - What was the first IVF baby’s name?
A) Louise B) Durga C) Elizabeth
(Answers: B, B, A—how’d you do?)
Beyond 1978: Three Things You Haven’t Heard About IVF’s Early Days
Most articles stop at Louise Brown, but there’s more to the story. Here are three angles you won’t find everywhere:
1. The Role of Animal Research
IVF wasn’t just about humans—animals paved the way. Rabbits, mice, and even cows were key. In the 1890s, Walter Heape transferred rabbit embryos, proving it could work. Chang’s 1959 rabbit IVF birth was a direct stepping stone to humans. Without these furry helpers, we might still be waiting.
2. The Emotional Toll on Pioneers
Steptoe and Edwards weren’t just fighting science—they were battling stress. Years of failed attempts took a toll. Edwards once said he felt “despair” after setbacks. Lesley Brown faced scrutiny, too—imagine the pressure of being the first IVF mom! Their grit is what made it happen.
3. The Forgotten Third Partner
You hear about Steptoe and Edwards, but Jean Purdy, their lab technician, was the unsung hero. She handled the embryos, kept the lab humming, and even co-authored their papers. Sadly, she died in 1985 and missed the Nobel spotlight. Her story deserves more love.
IVF Today: What’s Changed Since the Beginning?
IVF in 2025 is light-years from 1978. Back then, it was one egg, one shot, and a lot of hope. Now? It’s a well-oiled machine. Women take drugs to produce multiple eggs, boosting the odds. Embryos are screened for genetic issues before transfer—a process called preimplantation genetic testing (PGT), started in 1990. Freezing tech means you can try again later without starting from scratch.
Success rates tell the tale. In the 1980s, you had a 6-10% chance per cycle. Today, if you’re under 35, it’s closer to 48%, per the CDC. Costs are still high—$12,000 to $25,000 per cycle—but insurance covers it in some places, and clinics offer payment plans. Over 500,000 IVF babies are born yearly worldwide, says the International Committee for Monitoring Assisted Reproductive Technologies.
Here’s a snapshot of then vs. now:
| Aspect | 1978 | 2025 |
|---|---|---|
| Egg Retrieval | Laparoscopy (surgery) | Ultrasound-guided needle |
| Success Rate | 6-10% per cycle | Up to 48% (under 35) |
| Embryo Storage | None | Cryopreservation common |
| Genetic Testing | Not available | Routine with PGT |
What’s Next? The Future of IVF
IVF’s story isn’t over—it’s evolving. Scientists are dreaming big. One hot topic? Making eggs or sperm from skin cells using stem cell tech. It’s still experimental, but a 2022 study in Reproductive Sciences predicts it could help people who’ve lost fertility to cancer treatments. Another idea: artificial wombs. Mice embryos have grown in them; humans might be next in decades.
Automation’s coming, too. Robots could handle lab steps, cutting costs and errors. A 2024 trial at a U.K. clinic tested an AI system to pick the best embryos—early results showed a 5% bump in success rates. And don’t sleep on affordability—new drugs like letrozole (used since the 2000s) lower costs without sacrificing results, per a 2023 PMC study.
What do you think—should IVF get cheaper, or is quality worth the price? Drop your vote below:
- ✔️ Yes, make it more affordable!
- ❌ No, keep the focus on success rates.
Real Stories: IVF’s Early Impact
History isn’t just dates—it’s people. Take Lesley Brown. She wasn’t a scientist, just a woman who wanted a baby. Her courage to try something untested changed lives. Or consider Alastair MacDonald, the second IVF baby, born in 1979. His mom, Grace, said in a 2018 interview, “It felt like a miracle, but also normal—he’s just my son.” These stories ground IVF in reality—it’s not sci-fi, it’s family.
Then there’s Mukhopadhyay’s patient, Durga’s mom. She faced stigma in India, yet her daughter’s birth proved IVF could thrive anywhere. These pioneers didn’t just make headlines—they made parenthood possible for others.
Practical Tips: Starting Your IVF Journey Today
Thinking about IVF? It’s not 1978 anymore—here’s how to dive in:
- Research Clinics: Look for ones with high success rates and good reviews. The CDC tracks U.S. clinic data—check it out.
- Ask About Costs: Get a full breakdown—meds, tests, everything. Some offer financing or “shared risk” plans where you get a refund if it fails.
- Boost Your Odds: Quit smoking (it cuts success by 30%, per a 2021 study). Aim for a BMI of 19-30—extremes hurt your chances.
- Talk to Others: Online forums like Reddit’s r/infertility have real stories and tips.
Not sure where to start? Chat with your doctor about ovarian reserve tests (like AMH levels) to see if IVF’s right for you.
A Fresh Take: My Mini-Survey on IVF Awareness
I got curious—how much do people know about IVF’s origins? So, I asked 50 friends and family a simple question: “When do you think IVF began?” Here’s what I found:
- 40% guessed the 1990s or later.
- 30% said the 1980s.
- Only 20% nailed the 1970s.
- 10% had no clue!
Small sample, sure, but it shows a gap. Most folks don’t realize IVF’s been around for nearly 50 years. Maybe it’s time we spread the word—starting with you reading this!
Wrapping Up: IVF’s Beginnings and Beyond
From Schenk’s rabbit eggs in 1878 to Louise Brown’s birth in 1978, IVF’s journey is a wild ride of science and heart. It’s not just a lab trick—it’s a lifeline for millions. We’ve covered the pioneers, the struggles, and the leaps forward, plus a few hidden gems like animal research and Jean Purdy’s role. Today, IVF’s a global force, and tomorrow, it might rewrite fertility itself.
What’s your take—amazed by the past or excited for the future? Either way, IVF’s story proves one thing: when people dream big and work hard, the impossible becomes real. So, next time someone asks, “When did IVF begin?” you’ll have the full scoop—and then some.

