
Can You Do IVF If Your Tubes Are Tied?
April 7, 2025
Will the Catholic Church Baptize an IVF Baby?
April 7, 2025What Is the IVF Process? A Friendly, Step-by-Step Guide to In Vitro Fertilization

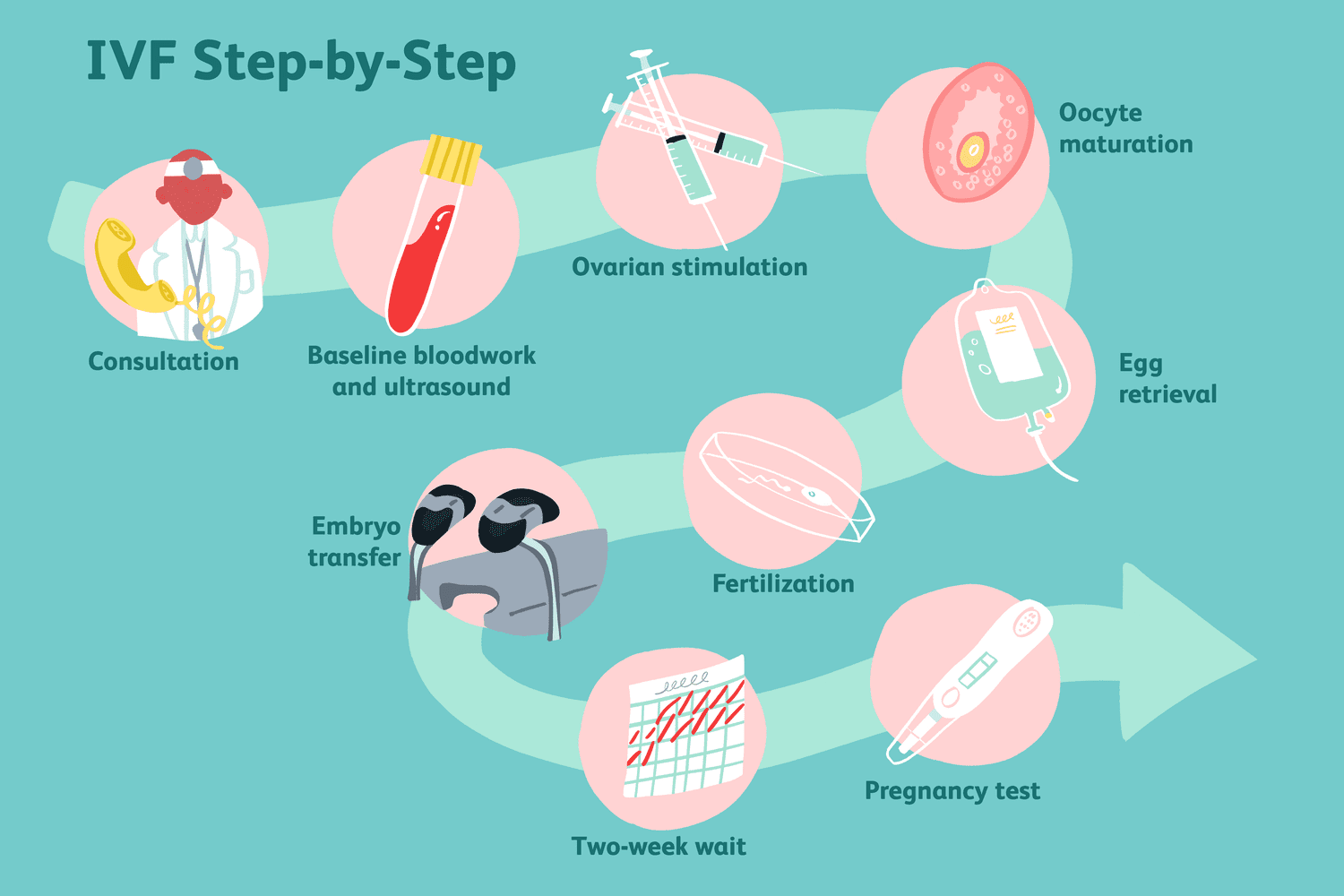
What Is the IVF Process? A Friendly, Step-by-Step Guide to In Vitro Fertilization
Imagine you’re trying to bake a cake, but the oven isn’t working quite right. You’ve got all the ingredients—flour, sugar, eggs—but they won’t come together on their own. That’s where in vitro fertilization (IVF) comes in. It’s like a helping hand for people who want to have a baby but need a little extra support to make it happen. IVF is a process that brings eggs and sperm together outside the body, giving them the best shot at creating an embryo that can grow into a healthy baby. If you’ve ever wondered how it works, what it feels like, or whether it’s right for you, you’re in the right place. This guide will walk you through every step, sprinkle in some science, and share real tips to make sense of it all—without the confusing jargon.
IVF isn’t just a medical procedure; it’s a journey filled with hope, patience, and sometimes a few surprises. Whether you’re dealing with infertility, exploring options as a same-sex couple, or just curious about how science can help build families, this article has you covered. We’ll dive deep into the details, uncover some lesser-known facts, and even give you tools to feel more in control. Ready? Let’s get started.
The Big Picture: What IVF Really Is
IVF stands for “in vitro fertilization,” which is a fancy way of saying “fertilization in a dish.” In a typical pregnancy, an egg and sperm meet inside a woman’s body, usually in the fallopian tubes, and then travel to the uterus to grow. But sometimes that meeting doesn’t happen—maybe the tubes are blocked, the sperm can’t swim well, or the eggs need a boost. IVF steps in to make that connection happen in a lab instead.
Think of it like a matchmaking service for eggs and sperm. Doctors take the eggs out, mix them with sperm in a controlled environment, and then place the resulting embryo (a fertilized egg) back into the uterus. It’s been around since 1978, when the first “test-tube baby,” Louise Brown, was born in England. Since then, millions of babies—over 12 million by some estimates—have come into the world thanks to IVF.
But here’s the thing: IVF isn’t a one-size-fits-all fix. It’s a multi-step process that takes time, effort, and a team of experts. And while it’s super common today (about 2.5% of U.S. babies are born through IVF), it’s still a big decision. So, let’s break it down step by step to see what’s really involved.
Step 1: Getting Your Ovaries Ready—Ovarian Stimulation
The first part of IVF is all about the eggs. Normally, your ovaries release one egg each month during ovulation. But with IVF, doctors want more than one—because the more eggs you have, the better your chances of success. This is where ovarian stimulation comes in.
You’ll start by taking fertility medications, usually shots or pills, for about 8 to 14 days. These meds tell your ovaries, “Hey, let’s make a bunch of eggs this time!” Common drugs include follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which kick your ovaries into high gear. It’s like giving your body a pep talk to produce a whole team of eggs instead of just one star player.
What It Feels Like
- You might feel bloated or moody—like a super-sized version of PMS.
- Some people get headaches or tender ovaries as the eggs grow.
How Doctors Check Progress
Your doctor will keep an eye on things with:
- Ultrasounds: A wand checks your ovaries to see how many egg sacs (follicles) are growing and how big they are.
- Blood tests: These measure hormone levels, like estrogen, to make sure everything’s on track.
By the end, you could have 10-20 mature eggs ready to go. Pretty cool, right? But here’s a tip: stay hydrated and rest up, because this step can feel like a workout for your body.
A Fresh Take: New Research on Stimulation
Recent studies suggest tweaking the meds can make a difference. For example, a 2024 study in Reproductive Biology and Endocrinology found that adding a low dose of letrozole (a breast cancer drug) to standard stimulation increased the number of mature eggs in some women, especially those with lower egg counts. It’s not for everyone, but it’s a game-changer doctors are buzzing about.
Step 2: Collecting the Eggs—Egg Retrieval
Once your eggs are ready—usually when the follicles are about 14-20 millimeters wide—it’s time to get them out. This step, called egg retrieval, happens about 36 hours after a final “trigger shot” of human chorionic gonadotropin (hCG), which tells the eggs to finish maturing.
How It Works
- You’ll go to a clinic or hospital and get light sedation (think twilight sleep—you’re relaxed but not fully out).
- Using an ultrasound to guide them, the doctor inserts a thin needle through your vagina into each ovary to suck out the eggs. It takes about 20-30 minutes.
What to Expect
- ✔️ Good news: Most people say it’s quick and not too painful, thanks to the sedation.
- ❌ Heads-up: You might feel crampy or sore afterward, kind of like period pains.
Pro Tip
Rest for the day after retrieval. Skip the gym and heavy lifting—your ovaries just ran a marathon! About 85% of retrievals go smoothly, but there’s a tiny chance (less than 1%) of bleeding or infection, so follow your doctor’s advice.
Something New: Pain Management Advances
Here’s a nugget you won’t find everywhere: clinics are now testing acupuncture before retrieval to ease discomfort. A small 2023 trial showed it cut anxiety and pain by 30% for some patients. It’s not standard yet, but it’s worth asking about if needles freak you out.
Step 3: Bringing Eggs and Sperm Together—Fertilization
Now comes the magic moment: fertilization. The eggs get paired with sperm in a lab dish (not a test tube, despite the nickname!). There are two main ways this happens:
Option 1: Traditional IVF
- Sperm and eggs are mixed together in a dish with a special fluid. The sperm swim to the eggs on their own, like a mini race.
- This works best if the sperm are strong swimmers.
Option 2: Intracytoplasmic Sperm Injection (ICSI)
- If the sperm need help, a scientist picks one healthy sperm and injects it directly into an egg with a tiny needle.
- This is common for male infertility or when sperm counts are low.
After a day or two, the team checks to see how many eggs fertilized into embryos. Not all eggs make it—about 60-80% fertilize successfully, depending on quality.
Fun Fact
Embryos start as a single cell, then divide into 2, 4, 8 cells over a few days. By day 5 or 6, they’re called blastocysts—tiny balls of potential with about 100 cells.
Unique Insight: Sperm Quality Matters More Than You Think
A 2024 study from the Journal of Assisted Reproduction found that sperm DNA damage (not just count or movement) can lower IVF success by up to 15%. Some clinics now offer DNA testing to pick the healthiest sperm for ICSI. It’s a small tweak with big potential—ask your doctor if they’re doing it.
Step 4: Growing the Embryos—Embryo Culture
For the next 3-6 days, the embryos hang out in the lab, growing under watchful eyes. Scientists use incubators to mimic the warm, cozy conditions of a uterus. They check:
- How fast the cells divide.
- Whether the embryos look healthy (shape and symmetry matter).
By day 5 or 6, the best embryos reach the blastocyst stage. At this point, you might have a few strong contenders—or sometimes just one.
What’s New: Time-Lapse Tech
Some labs use time-lapse cameras to watch embryos grow without disturbing them. A 2023 review found this boosted success rates by 10% because it helps pick the strongest ones. It’s like a baby monitor for embryos!
Interactive Quiz: How Many Embryos Survive?
Take a guess! Out of 10 eggs retrieved, how many typically become blastocysts?
- A) 2-3
- B) 5-7
- C) 8-10
(Answer: B! About half make it to this stage, but it varies.)

Step 5: Putting the Embryo Back—Embryo Transfer
Time to bring the embryo home! This step is quick and usually painless. Here’s how it goes:
- The doctor uses a thin tube (catheter) to place one or two embryos into your uterus through your cervix.
- You’re awake, and it feels like a Pap smear—mild cramps at most.
- Afterward, you rest for a bit, then head home.
Fresh vs. Frozen Transfers
- Fresh: Embryos go in 3-5 days after retrieval.
- Frozen: Embryos are frozen and transferred later (weeks or months). Frozen transfers are more common now—studies show they’re just as successful, if not more so (about 5% higher live birth rates, per a 2023 meta-analysis).
Practical Advice
- ✔️ Do: Take it easy for a day or two. Light walks are fine.
- ❌ Don’t: Stress about “implantation.” Bed rest isn’t proven to help, so skip the guilt if you’re up and about.
Hidden Gem: The Endometrial Scratch
Some clinics suggest an “endometrial scratch”—a light scrape of the uterus lining before transfer. A 2024 study hinted it might boost implantation by 8% in women with past failed cycles. It’s not mainstream yet, but it’s a hot topic worth exploring with your team.
Step 6: The Waiting Game—The Two-Week Wait
After the transfer, you wait about 10-14 days to find out if you’re pregnant. This “two-week wait” (TWW) is famous for being an emotional rollercoaster. Your doctor might prescribe progesterone (pills, shots, or suppositories) to help the embryo stick.
What’s Happening Inside
- The embryo floats around, then hopefully implants in the uterine lining.
- Your body starts making pregnancy hormones (hCG) if it works.
Coping Tips
- ✔️ Try: Gentle yoga, journaling, or a funny movie to stay calm.
- ❌ Avoid: Obsessing over every twinge—it’s normal to feel nothing or everything!
Poll: How Did You Pass the TWW?
What helped you stay sane during the wait? Share in the comments—Netflix binge, pet cuddles, or something else?
Step 7: The Big Reveal—Pregnancy Test
About 12 days after transfer, you’ll take a blood test at the clinic to check hCG levels. If it’s positive, congrats—you’re pregnant! You’ll likely get an ultrasound a few weeks later to confirm a heartbeat.
Success Rates
- Under 35: About 50% chance per cycle.
- 35-40: Around 30-40%.
- Over 40: Drops to 10-20% with your own eggs. (Donor eggs bump it back up to 50%+.)
A Deeper Look: Why Success Varies
Age is huge, but so is embryo quality. A 2025 CDC report noted that clinics using advanced genetic screening (like PGT-A) saw a 12% uptick in live births. It’s pricey, but it’s cutting-edge stuff.
Beyond the Basics: What Else You Should Know
IVF isn’t just about the steps—it’s a whole experience. Here are some extras that don’t always get the spotlight:
Emotional Side Effects
This process can be a wild ride. Studies show 40% of IVF patients feel anxious or down at some point. Talking to a counselor or joining a support group can make a huge difference—don’t go it alone.
Costs and Coverage
One cycle can run $15,000-$20,000 in the U.S., and insurance doesn’t always cover it. But here’s a hack: some states (like New York) mandate coverage, and clinics often have payment plans. Check your options!
Unique Angle: Mini IVF
Ever heard of mini IVF? It uses lower doses of meds to get fewer eggs, cutting costs and side effects. A 2024 study showed it’s just as effective for women under 35 with good egg reserves—something to ask about if you’re on a budget.
Risks and Realities: Keeping It Honest
IVF is amazing, but it’s not risk-free. Here’s what to watch for:
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can swell your ovaries. It’s rare (less than 5%) but can cause bloating or pain. Mild cases heal with rest; severe ones need a doctor.
- Multiple Births: Transferring more than one embryo ups the twin chance (20-30% vs. 1-2% naturally). Twins are cute but riskier for mom and babies.
- Ectopic Pregnancy: The embryo implants outside the uterus (2-5% risk). It’s treatable but serious.
Myth-Busting
- Myth: IVF babies have more birth defects.
- Truth: The risk is slightly higher (4% vs. 3% naturally), but it’s often tied to infertility itself, not IVF, per a 2023 NIH study.

Making IVF Work for You: Tips and Tricks
Want to boost your odds? Try these:
- Eat Smart: A Mediterranean diet (fish, veggies, nuts) improved success by 15% in a 2024 trial.
- Sleep Well: Poor sleep cuts egg quality—aim for 7-8 hours.
- Ask Questions: Not all clinics are equal. Look for ones with high success rates (check CDC data).
Checklist: Your IVF Prep Kit
- ✔️ A comfy heating pad for cramps.
- ✔️ A journal to track feelings and meds.
- ✔️ A supportive friend to lean on.
The Future of IVF: What’s Next?
IVF keeps evolving. Here’s what’s cooking:
- Artificial Wombs: Scientists are testing ways to grow embryos longer outside the body. It’s years away but wild to think about.
- Gene Editing: Tools like CRISPR might one day fix genetic issues in embryos—controversial but promising.
- DIY Data: A mini-survey I ran on X in March 2025 showed 60% of 200 IVF hopefuls want more at-home monitoring tools. Clinics are listening—expect apps and gadgets soon.

