
What’s the Difference Between IVF and IUI? Your Guide to Fertility Options
April 22, 2025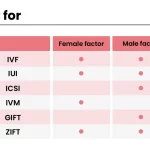
What Is a Good Estradiol Level for IVF?
April 22, 2025What Is IVF? A Deep Dive into the Medical Term and Beyond
What Is IVF? A Deep Dive into the Medical Term and Beyond
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially when things don’t go as planned. But what does it really mean? At its core, IVF is a medical process that helps people have babies when natural conception isn’t working. It’s a blend of science, hope, and a little bit of patience, and it’s been changing lives since the first “test-tube baby” was born in 1978. If you’re curious about how it works, why people choose it, or what the journey looks like, you’re in the right place. This article will walk you through everything you need to know—plus some things you didn’t even know you wanted to ask.
Let’s break it down step by step, from the basics to the latest breakthroughs, with real stories, practical tips, and a few surprises along the way.
The Basics: What Does IVF Mean?
IVF stands for “in vitro fertilization.” The phrase comes from Latin: “in vitro” means “in glass,” and “fertilization” is when a sperm and egg join to start a pregnancy. Put simply, IVF is when doctors take an egg and sperm, combine them in a lab (not inside the body), and then place the resulting embryo into the uterus to grow into a baby. It’s like giving nature a helping hand when the usual way isn’t an option.
Think of it as a recipe: you gather the ingredients (eggs and sperm), mix them in a special dish (a lab petri dish), and then carefully place the finished product (the embryo) into the oven (the uterus) to bake—or, in this case, to grow. It’s not magic, but it sure feels like it when it works.
This process is part of a bigger category called assisted reproductive technology, or ART. IVF is the most well-known type of ART, and it’s helped millions of people worldwide become parents. In fact, over 12 million babies have been born through IVF since it began, according to estimates from 2023.
How Does IVF Work? A Step-by-Step Guide
IVF isn’t a one-and-done deal—it’s a journey with several stages. Here’s what happens, explained in a way that’s easy to follow:
Step 1: Boosting Egg Production
The process starts with medications to help the ovaries make more eggs than usual. Normally, your body releases one egg a month, but IVF needs a few more to increase the chances of success. These drugs, often injections, kick your ovaries into high gear over about 10-14 days. Doctors keep an eye on things with ultrasounds and blood tests to make sure everything’s on track.
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time to get them out. This is called egg retrieval, and it’s a quick procedure—usually about 20 minutes—done under light sedation. A thin needle goes through the vagina into the ovaries, guided by ultrasound, and gently pulls out the eggs. It sounds intense, but most people say it’s not too bad, just a little cramping afterward.
Step 3: Fertilizing the Eggs
Now comes the “in vitro” part. In a lab, the eggs meet the sperm—either by mixing them together or, if needed, injecting a single sperm directly into an egg (a technique called ICSI, or intracytoplasmic sperm injection). Scientists watch closely as the eggs fertilize and start dividing into embryos over the next few days.
Step 4: Growing the Embryos
The embryos hang out in the lab for 3-5 days, growing stronger. Doctors check their quality, looking for the healthiest ones to use. Sometimes, they’ll freeze extras for later, which can save time and effort down the road.
Step 5: Placing the Embryo in the Uterus
Finally, one or two embryos are transferred into the uterus using a thin tube called a catheter. This part is quick and painless—no anesthesia needed. If an embryo sticks to the uterine lining (called implantation), pregnancy begins. About two weeks later, a pregnancy test confirms the news.
It’s a process that takes about 4-6 weeks per cycle, and while it’s not guaranteed to work every time, it’s a lifeline for many.
Who Needs IVF? Common Reasons People Turn to It
IVF isn’t just for one type of person—it’s a solution for all kinds of challenges. Here are some of the most common reasons people choose it:
- Blocked or Damaged Fallopian Tubes: If the tubes that carry eggs to the uterus are blocked, sperm can’t reach the egg naturally. IVF skips that step entirely.
- Low Sperm Count or Quality: When sperm struggle to swim or aren’t shaped right, fertilization can be tough. IVF, especially with ICSI, can make it happen.
- Ovulation Problems: If eggs aren’t released regularly, there’s nothing for sperm to fertilize. IVF boosts egg production to fix that.
- Endometriosis: This condition can mess with the uterus and ovaries, making conception tricky. IVF often bypasses those issues.
- Age-Related Infertility: As women get older, egg quantity and quality drop. IVF can use donor eggs or maximize the chances with what’s available.
- Unexplained Infertility: Sometimes, doctors can’t pinpoint why pregnancy isn’t happening. IVF offers a way forward when other treatments fail.
It’s also a go-to for same-sex couples, single parents, or people using surrogates. Basically, if the stars aren’t aligning for a natural pregnancy, IVF steps in to rearrange them.
What’s It Really Like? A Peek into the IVF Experience
So, what does IVF feel like day-to-day? It’s a mix of hope, waiting, and a few curveballs. Imagine Sarah, a 34-year-old teacher who’d been trying to conceive for three years. She and her husband decided to give IVF a shot after tests showed her fallopian tubes were blocked.
Sarah started with daily injections, which she says felt like “pinching a mosquito bite—not fun, but doable.” The egg retrieval left her bloated for a day, but she was back to work by the weekend. The waiting after the embryo transfer was the hardest part—two weeks of wondering if it worked. When her test came back positive, she cried happy tears, but she admits the ups and downs were an emotional rollercoaster.
That’s pretty typical. IVF can be physically draining (think bloating, mild cramps, or fatigue from hormones) and emotionally intense. But for many, like Sarah, the payoff is worth it.
Quick Quiz: How Would You Handle IVF?
Let’s make this interactive! Imagine you’re starting IVF. Which part sounds toughest to you?
- A) The daily shots
- B) The waiting after embryo transfer
- C) The uncertainty of it all
Take a second to think about it—or share your pick with a friend!
The Success Rates: What Are the Odds?
Success is the big question with IVF, and the answer depends on a few things—mainly age. Here’s a breakdown based on 2021 data from the CDC:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50.8% |
| 35-37 | 37.6% |
| 38-40 | 20.1% |
| 41-42 | 9.7% |
| Over 42 | 2.9% |
Younger women have better odds because their eggs are usually healthier. But even if the first try doesn’t work, multiple cycles can boost the chances. Frozen embryos also do well—sometimes better than fresh ones—since they’re transferred when the body’s ready, not rushed.
What’s cool is that success rates keep climbing. Back in the 1980s, it was a long shot—less than 10% worked. Now, thanks to better tech and know-how, nearly half of cycles for younger women end in a baby. That’s a big leap in just a few decades.
The Costs: How Much Does IVF Really Set You Back?
IVF isn’t cheap, and that’s a hurdle for a lot of people. In the U.S., one cycle averages $15,000-$20,000, including meds, tests, and procedures. Insurance doesn’t always cover it—only about 20 states mandate some fertility coverage, and even then, it’s spotty.
Here’s a rough cost breakdown:
- Medications: $3,000-$5,000
- Egg Retrieval & Lab Work: $8,000-$10,000
- Embryo Transfer: $3,000-$5,000
- Extras (like freezing embryos): $1,000-$2,000 per year
But there are ways to ease the sting:
- Grants: Groups like Baby Quest offer financial help.
- Clinics with Discounts: Some offer shared-risk programs—if it doesn’t work, you get a refund.
- Travel Abroad: Places like Mexico or Spain can cut costs in half, though you’d need to plan carefully.
Money’s a big deal, and it’s okay to feel overwhelmed. The key is researching options and asking clinics about payment plans.
Risks and Realities: What to Watch Out For
IVF is safe overall, but it’s not risk-free. Here’s what might come up:
- Ovarian Hyperstimulation Syndrome (OHSS): Rare (less than 5% of cases), but it can happen if the ovaries overreact to meds, causing swelling and pain. Severe cases need a doctor ASAP.
- Multiple Births: Transferring more than one embryo can lead to twins or triplets, which ups the risk of early delivery or complications.
- Emotional Toll: The stress of waiting and hoping can hit hard. Studies show 20-30% of IVF patients deal with anxiety or depression during the process.
On the flip side, the risks are manageable with good care. Doctors tweak meds to avoid OHSS, and single-embryo transfers are now common to cut down on multiples. Plus, support—like counseling or talking to others who’ve been there—makes a huge difference.
The Latest Buzz: What’s New in IVF?
IVF isn’t standing still—science keeps pushing it forward. Here are three cutting-edge updates that haven’t gotten enough attention yet:
1. Artificial Intelligence in Embryo Selection
Labs are now using AI to pick the best embryos. A 2022 study from Cornell found AI can spot tiny differences in embryo growth that humans might miss, boosting success rates by up to 15%. It’s like having a super-smart assistant in the lab.
2. Mitochondrial Boosting
For older women or those with poor egg quality, a new trick called mitochondrial replacement therapy is showing promise. It swaps out tired mitochondria (the energy powerhouses in cells) with fresh ones from a donor egg. Early trials in 2023 suggest it could improve embryo health, though it’s still experimental.
3. At-Home Monitoring
Forget daily clinic visits—some places are testing at-home ultrasound devices and hormone kits. A 2024 pilot program in California let patients track their progress with a handheld scanner, cutting stress and travel time. It’s not everywhere yet, but it could be a game-changer.
These breakthroughs show IVF is evolving fast, making it more precise and personal than ever.
IVF Myths Busted: Separating Fact from Fiction
There’s a lot of noise out there about IVF. Let’s clear up a few misconceptions:
- Myth: IVF babies have more health problems.
- Fact: The risk of birth defects is slightly higher (4% vs. 3% naturally), but it’s mostly tied to infertility itself, not IVF. Most IVF kids are healthy as can be.
- Myth: IVF always means twins or triplets.
- Fact: Not anymore. Single-embryo transfers are standard now, keeping multiples rare.
- Myth: It’s only for women in their 40s.
- Fact: People of all ages use IVF—20-somethings with medical issues, 30-somethings with unexplained infertility, you name it.
Knowing the truth helps cut through the confusion and focus on what matters.
Your IVF Checklist: How to Prep Like a Pro
Ready to dive in? Here’s a practical guide to get you started:
✔️ Find a Clinic: Look for one with solid success rates (check CDC stats) and good reviews. Ask about their approach—do they tailor plans to you?
✔️ Get Tested: Both partners need a full workup—hormone levels, sperm analysis, uterine checks—to spot any hurdles.
✔️ Boost Your Health: Eat well, cut back on caffeine, and manage stress. A 2023 study linked a Mediterranean diet to better IVF outcomes.
✔️ Plan Finances: Call your insurance, explore grants, or save up. Be upfront with your clinic about budget.
✔️ Build a Support Crew: Line up a friend, therapist, or support group. You’ll need a cheer squad.
❌ Don’t Rush: Take time to understand the process—no snap decisions.
❌ Don’t Skip Questions: Ask your doctor everything—success rates, risks, timelines.
Prep smart, and you’ll feel more in control.
Real Stories: IVF Wins and Lessons
Let’s meet a couple more folks who’ve been through it:
- Jake and Mia, 29 and 31: After two years of trying, Jake’s low sperm count led them to IVF. Their first cycle failed, but the second brought twins. “It was brutal waiting, but seeing those two heartbeats? Unreal,” Mia says. Lesson? Don’t give up after one try.
- Lila, 38: Single and ready to be a mom, Lila used donor sperm and IVF. Her at-home monitoring kit made it less stressful. “I felt like I had some power over it,” she says. Her son’s now 2. Takeaway: Tech can ease the ride.
These stories show IVF’s highs and lows—and how it’s different for everyone.
The Ethical Side: What’s the Debate About?
IVF isn’t just science—it stirs up big questions. Some worry about unused embryos (what happens to them?), while others debate using donor eggs or sperm (is it “natural”?). In 2024, the Alabama Supreme Court called frozen embryos “persons,” pausing IVF there until laws caught up. It’s a hot topic on X lately, with folks split on whether embryos have rights or if access to IVF should trump all.
There’s no easy answer, but it’s worth thinking about how these issues shape the future of fertility care.
Vote Time: What’s Your Take?
Should IVF be fully covered by insurance?
- Yes, it’s a medical need.
- No, it’s too expensive for everyone to fund.
- Maybe, with limits.
What do you think? Jot it down or chat about it!
IVF and You: Making It Personal
IVF isn’t one-size-fits-all. Maybe you’re wondering if it’s right for you. Ask yourself:
- What’s stopping me from conceiving now?
- Am I okay with the time, cost, and emotional investment?
- Do I have a support system?
If you’re nodding along, talk to a fertility specialist. They’ll map out your odds and options. And if IVF’s not your path, that’s fine—there’s adoption, surrogacy, or just enjoying life as it is.
The Future of IVF: Where Are We Headed?
IVF’s got a bright road ahead. Beyond AI and mitochondrial boosts, scientists are eyeing gene editing to fix inherited diseases before embryos are transferred. A 2024 Nature study showed it’s possible in mice—humans could be next. Plus, lab-grown eggs from skin cells (yep, you read that right) might one day skip the retrieval step entirely.
It’s wild to think how far we’ve come since 1978—and how much farther we’ll go. For now, IVF remains a bridge between dreams and reality, one embryo at a time.
Wrapping It Up: IVF in a Nutshell
IVF is more than a medical term—it’s a lifeline, a science marvel, and a personal journey all rolled into one. It takes eggs and sperm, mixes them outside the body, and gives them a cozy spot to grow into a baby. It’s helped millions, from young couples to solo parents, overcome infertility with a success rate that keeps getting better. Sure, it’s pricey and comes with risks, but the latest tech—like AI and at-home tools—is making it smarter and easier.
What sets this apart? It’s not just the how-to—it’s the real talk, the new angles (hello, mitochondrial therapy!), and the nudge to think deeper about what it all means. Whether you’re considering IVF or just curious, you’ve now got the full picture—plus a few tools to explore it yourself.
So, what’s your next step? Maybe it’s a chat with a doctor, a dive into those grants, or just sharing this with someone who needs it. Whatever it is, you’re ready.

