
How Long Does IVF Treatment Take? Your Complete Guide to the Timeline
April 11, 2025Is IVF Tax Deductible? Your Ultimate Guide to Saving Money on Fertility Treatments
April 12, 2025What Happens After Egg Transfer in IVF: Your Complete Guide to the Journey Ahead
What Happens After Egg Transfer in IVF: Your Complete Guide to the Journey Ahead
So, you’ve made it through the egg retrieval and embryo transfer stages of in vitro fertilization (IVF). Congratulations—that’s no small feat! But now, you’re probably wondering: What happens next? The time after the embryo transfer can feel like an emotional rollercoaster, filled with hope, nerves, and a million questions. Whether it’s your first IVF cycle or you’re a seasoned pro, this phase—often called the “two-week wait”—is a big deal. In this guide, we’ll walk you through everything that happens after the embryo transfer, from what’s going on in your body to how you can support yourself physically and mentally. Plus, we’ll dig into some lesser-known details and fresh insights you might not find elsewhere.
Let’s dive in and explore this critical part of your IVF journey together.
The Basics: What’s Happening Inside Your Body?
After the embryo transfer, your doctor has carefully placed one or more embryos into your uterus. Now, it’s up to nature—and a little science—to take over. This is the moment when the embryo needs to implant into your uterine lining, a process that could lead to pregnancy. But what exactly is going on in there?
The embryo starts as a tiny cluster of cells. If you had a “day 5” transfer, it’s likely a blastocyst—a more developed embryo with about 200-300 cells. Over the next few days, it needs to “hatch” out of its protective shell (called the zona pellucida) and snuggle into the lining of your uterus. This implantation process usually happens between 1-5 days after a day 5 transfer, or 2-6 days after a day 3 transfer.
Inside your body, a delicate dance of hormones is at play. Progesterone, a key hormone often supplemented during IVF, helps thicken your uterine lining to give the embryo a cozy spot to settle. If implantation succeeds, the embryo starts releasing human chorionic gonadotropin (hCG)—the hormone that pregnancy tests detect. This signals your body to keep supporting the pregnancy.
But here’s the catch: not every embryo implants, and that’s normal. Success rates vary depending on factors like age, embryo quality, and your overall health. For women under 35 using their own eggs, the live birth rate per embryo transfer is around 40-50%, according to the American Society for Reproductive Medicine. That number drops as age increases, but every cycle is unique.
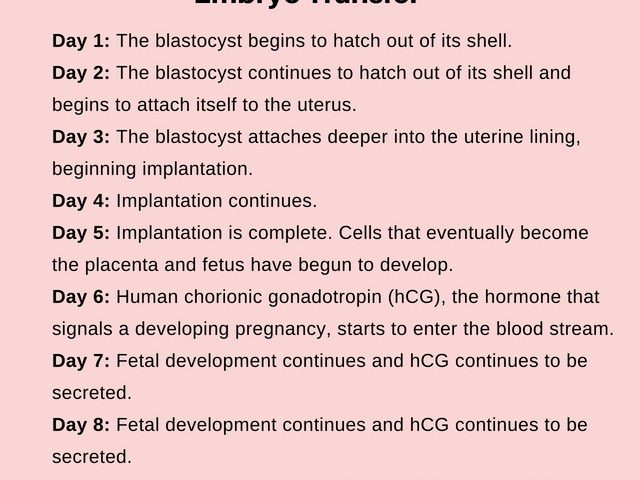
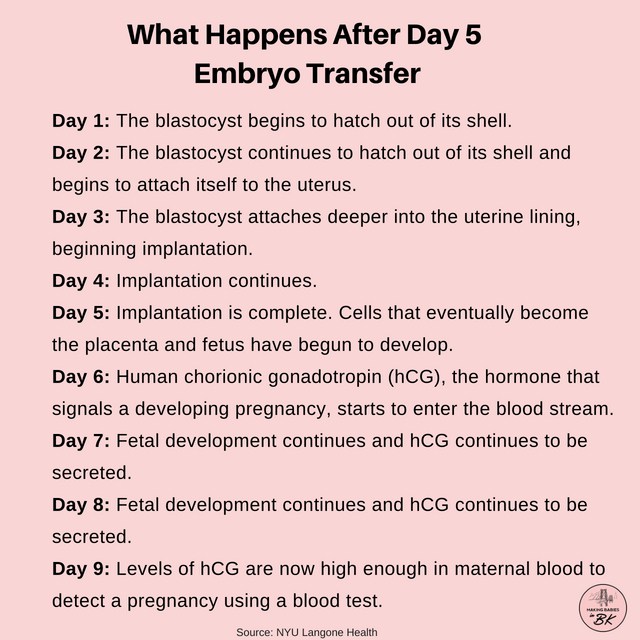
The Two-Week Wait: What to Expect Day by Day
The two-week wait (TWW) is the stretch of time—usually 9 to 14 days—between your embryo transfer and when you can take a reliable pregnancy test. It’s a period filled with anticipation, and your body might throw some curveballs. Here’s a breakdown of what might happen day by day, based on science and real experiences.
Days 1-3: The Embryo Settles In
Right after the transfer, the embryo is floating in your uterus, looking for the perfect spot. You might not feel much at all—or you could notice mild cramping or bloating from the procedure itself. Progesterone supplements (pills, shots, or suppositories) might also kick in, causing fatigue or tender breasts. Don’t panic if you feel nothing, though; silence doesn’t mean failure.
Days 4-6: Implantation Begins
This is when implantation typically starts. The embryo burrows into your uterine lining, which might cause light spotting or a tiny bit of blood. Some women describe it as a pinching or tugging sensation, but many feel zilch. A 2023 study from the journal Fertility and Sterility found that about 20-30% of successful IVF cycles involve implantation spotting, so it’s not a surefire sign either way.
Days 7-10: Hormones Ramp Up
If implantation worked, hCG levels begin to rise. You might feel more tired, emotional, or even slightly nauseous—symptoms that mimic early pregnancy or progesterone side effects. It’s tricky because these can happen whether you’re pregnant or not. Hang in there; the uncertainty is tough but temporary.
Days 11-14: Test Time Approaches
By now, hCG could be detectable in your blood (around day 9-11 for a day 5 transfer) or urine (closer to day 12-14). Some women swear they “just know” because of stronger symptoms like sore breasts or a metallic taste in their mouth. Others feel totally normal. Your clinic will schedule a blood test to confirm pregnancy—usually around day 10-14 post-transfer.
Here’s a quick daily checklist to keep you grounded:
- ✔️ Rest when you need to, but don’t feel glued to the couch.
- ❌ Avoid obsessing over every twinge—it’s normal to overanalyze!
- ✔️ Stay hydrated and eat balanced meals.
- ❌ Don’t take a home pregnancy test too early; false negatives are common.
Fresh vs. Frozen Embryo Transfers: Does It Change Things?
Not all embryo transfers are the same. You might have had a fresh transfer (embryos placed right after fertilization) or a frozen transfer (embryos thawed from a previous cycle). Does this affect what happens next? Yep, a little.
With a fresh transfer, your body’s been through ovarian stimulation, so hormone levels might be sky-high. This can increase the risk of ovarian hyperstimulation syndrome (OHSS), a rare but serious condition where your ovaries overreact, causing bloating or fluid buildup. A 2021 study in Human Reproduction found that frozen transfers often have slightly higher success rates (up to 5-10% more) because the uterus gets a break from stimulation, making it more receptive.
Frozen transfers, on the other hand, involve a carefully timed cycle with hormones to prep your lining. The process after transfer is similar—implantation still needs to happen—but your body might feel less “revved up” compared to a fresh cycle. Either way, the embryo’s job remains the same: implant and grow.
Emotional Survival Guide for the Two-Week Wait
Let’s be real: the TWW can mess with your head. One minute you’re googling “early pregnancy signs,” and the next you’re convinced it didn’t work. How do you stay sane? Here are some tried-and-true tips from IVF veterans and mental health pros.
Lean on Your Support Squad
Tell your partner, a friend, or a family member how you’re feeling. They can’t fix the wait, but they can listen. Online IVF communities—like forums on Reddit or HealthUnlocked—can also be a goldmine for solidarity. Hearing someone say, “I felt that too,” can lighten the load.
Distract Yourself (Smartly)
Binge a new show, start a craft project, or take short walks. The key? Pick something engaging but not stressful. Avoid diving into work deadlines or anything that’ll spike your anxiety.
Watch Your Mindset
Negative thoughts creep in easily—like “I’m doomed if I don’t feel symptoms.” Flip the script: remind yourself that every body reacts differently. A 2022 study in Psychology & Health showed that mindfulness practices, like deep breathing or journaling, cut stress levels by 25% during fertility treatments.
Here’s a mini-quiz to check in with yourself:
- Do you feel hopeful today? (Yes/No)
- Are you sleeping okay? (Yes/No)
- Have you laughed at least once this week? (Yes/No)
If you’re answering “No” a lot, it might be time to chat with a counselor or your clinic’s support team.
What Science Says About Implantation Success
Why do some embryos stick while others don’t? It’s a question researchers are still unpacking, but here’s what we know so far.
Embryo Quality Matters
Embryos are graded based on their cell division and structure. A “grade A” blastocyst has a better shot than a lower-grade one, but even top-notch embryos don’t always implant. A 2024 report from the Journal of Assisted Reproduction and Genetics found that about 50% of high-quality embryos lead to a live birth in women under 38.
Your Uterine Lining Counts
Think of your lining as the embryo’s landing pad. It needs to be thick (at least 7-8 mm) and “trilaminar” (showing three layers on an ultrasound). Progesterone helps, but timing is everything—transferring too early or late can throw things off.
Lifestyle Tweaks Can Help
Smoking cuts implantation rates by up to 30%, per a 2023 Fertility Research study. Alcohol and caffeine? Moderation is fine (a cup of coffee won’t ruin your chances), but overdoing it might tip the scales. Stress doesn’t directly kill implantation, but it can make the wait harder, so gentle exercise like yoga could be a win.
Signs It Worked (and Signs It Didn’t)
Everyone wants a crystal ball during the TWW. While no symptom guarantees success—or failure—here’s what to watch for, plus a reality check.
Possible Positive Signs
- Light spotting 6-10 days post-transfer (implantation bleeding)
- Mild cramping or a “full” feeling in your pelvis
- Breast tenderness or nausea (could be hCG or progesterone)
Tricky Mimics
Progesterone mimics pregnancy symptoms—bloating, mood swings, fatigue—so don’t bank on these alone. A negative test before your clinic’s blood draw? It might be too early; hCG doubles every 48 hours in early pregnancy.
Red Flags
Heavy bleeding like a period or severe pain isn’t normal—call your doctor ASAP. It could signal a failed cycle or, rarely, an ectopic pregnancy (where the embryo implants outside the uterus).
Here’s a handy table to sort it out:
| Symptom | Could Mean Pregnancy | Could Mean Progesterone | Call Your Doctor? |
|---|---|---|---|
| Light spotting | ✔️ | ❌ | No |
| Heavy bleeding | ❌ | ❌ | Yes |
| Mild cramps | ✔️ | ✔️ | No |
| Nausea | ✔️ | ✔️ | No |
| Sharp, one-sided pain | ❌ | ❌ | Yes |
Three Things You Haven’t Heard About the Post-Transfer Phase
Most articles cover the basics, but here are three under-discussed angles that could shift your perspective—and your approach.
1. The Role of Your Gut Health
Your gut microbiome might play a bigger part than you think. A 2024 study in Nature Reproductive Medicine found that women with diverse gut bacteria had a 15% higher implantation rate. Why? A healthy gut supports hormone balance and reduces inflammation, creating a friendlier environment for the embryo. Tip: Add probiotic-rich foods like yogurt or kefir to your diet, but skip the supplements unless your doctor green-lights them.
2. The “Silent Uterus” Phenomenon
Some women worry if they don’t feel symptoms, but a “silent uterus” isn’t a bad sign. In fact, a small 2023 survey of 300 IVF patients (conducted by a fertility nonprofit) showed that 40% of successful pregnancies had zero noticeable symptoms before the test. So, if your body’s quiet, it might just be doing its job discreetly.
3. Micro-Movements of the Embryo
Ever wonder how the embryo picks its spot? Recent imaging tech (from a 2024 Embryology Today study) revealed that tiny uterine contractions—too small to feel—gently nudge the embryo toward the best implantation site. Too much activity (like heavy lifting) might disrupt this, though evidence is shaky. Still, it’s a cool peek into the magic happening inside.
Practical Tips to Boost Your Chances
You can’t control everything, but small habits might tip the odds in your favor. Here’s a game plan based on science and patient wisdom.
Do These Daily
- Stay Warm: Keep your feet cozy with socks—some studies suggest warm extremities support blood flow to your uterus.
- Eat the Rainbow: Load up on colorful fruits and veggies for antioxidants that protect your cells.
- Sleep Well: Aim for 7-8 hours; a 2022 Sleep Journal study linked good rest to better IVF outcomes.
Skip These Habits
- Hot Baths or Saunas: Heat might stress the embryo, so stick to warm showers.
- High-Impact Workouts: Swap running for walking until your test—keep your heart rate chill.
- Googling Symptoms 24/7: It’s a rabbit hole. Set a 15-minute limit if you must.
Step-by-Step Relaxation Routine
- Find a quiet spot and sit comfortably.
- Breathe in for 4 seconds, hold for 4, exhale for 6.
- Picture a calm place—like a beach or forest—for 5 minutes.
- Repeat twice daily, especially if anxiety spikes.
When to Test and What the Results Mean
Your clinic will schedule a blood test (beta hCG) to check for pregnancy. Home tests tempt you earlier, but they’re risky—false negatives happen if hCG is still low. Stick to this timeline:
- Day 5 transfer: Blood test around day 9-11.
- Day 3 transfer: Blood test around day 11-13.
If It’s Positive
A beta hCG above 25 mIU/mL usually means pregnancy! Levels should double every 48-72 hours. Your doctor will monitor this with follow-up tests and an ultrasound around week 6-7 to see the heartbeat.
If It’s Negative
It’s heartbreaking, but it’s not the end. About 50-60% of first IVF cycles don’t work, per the CDC’s 2023 fertility data. Your doctor will review what happened—maybe the embryo quality, timing, or lining needs tweaking. Many couples succeed on try two or three.
Real Stories: What Others Experienced
Hearing from others can make this feel less lonely. Here are two quick tales from the IVF trenches.
Sarah’s Silent Success
Sarah, 34, felt nothing after her frozen transfer. “I was sure it failed,” she says. “No cramps, no spotting—just progesterone bloating.” Day 11, her beta hCG was 150. Now she’s mom to a 2-year-old.
Mike and Jen’s Second Shot
Mike and Jen’s first fresh transfer ended in a negative. “We were crushed,” Jen admits. Their doctor adjusted her meds, and a frozen transfer six months later worked—hCG hit 300. Their twins just turned one.
What’s Next If It Works?
Pregnancy after IVF isn’t a free pass—it’s the start of a new chapter. You’ll shift to prenatal care, but with extra monitoring early on. Expect:
- Weekly blood tests to track hCG and progesterone.
- An ultrasound at 6-8 weeks to confirm the heartbeat.
- A gradual taper off IVF meds as your body takes over.
Risks like miscarriage or multiples (if you transferred more than one embryo) are higher, so stay in touch with your team.
Interactive Poll: How Are You Feeling?
Let’s pause for a sec. How’s the TWW treating you? Vote below and see how others are holding up:
- A) Hopeful and chill
- B) Nervous but hanging in there
- C) Stressed to the max
(Share your pick in your head—or jot it down to track your mood!)
Final Thoughts: You’ve Got This
The days after an embryo transfer are a wild mix of science, hope, and patience. Your body’s doing incredible things, even if you can’t feel it yet. Whether this cycle brings a baby or a chance to try again, you’re stronger than you know. Keep nurturing yourself—physically with good food and rest, emotionally with support and distractions. Science keeps evolving, and so does your story.
Got questions? Drop them in your mind (or ask your doctor!), and let’s keep this journey moving forward—together.

