How Many Eggs Are Fertilized in IVF?
April 19, 2025
How Much Does IVF Cost in Pennsylvania?
April 19, 2025Does IVF Work? Your Guide to Understanding In Vitro Fertilization Success
Does IVF Work? Your Guide to Understanding In Vitro Fertilization Success
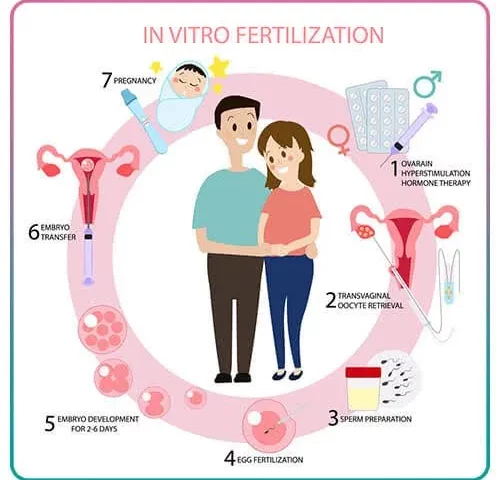
In vitro fertilization, or IVF, is a term you’ve probably heard if you’ve ever explored options for starting a family when natural conception isn’t working. It’s a process where doctors combine an egg and sperm outside the body, then place the resulting embryo into the uterus. But the big question on everyone’s mind is: Does it actually work? The short answer is yes, it can—but there’s so much more to unpack. Success isn’t guaranteed, and the journey can feel like a rollercoaster. Let’s dive into what makes IVF effective, who it works for, and what you can do to boost your chances, all while exploring the latest insights and real-life experiences.
What Is IVF and How Does It Work?
IVF is like a science experiment with a deeply human goal: helping people have a baby. It starts with stimulating the ovaries to produce multiple eggs, retrieving those eggs, fertilizing them with sperm in a lab, and then transferring an embryo (or sometimes two) into the uterus. If all goes well, the embryo implants, and a pregnancy begins. Simple, right? Not quite. Each step has its challenges, and success depends on a mix of biology, timing, and sometimes a little luck.
The process usually takes 3 to 6 weeks for one cycle, and it’s not a one-size-fits-all deal. Some people use their own eggs and sperm, while others rely on donors or even surrogates. There’s also a version called ICSI (intracytoplasmic sperm injection), where a single sperm is injected directly into an egg—super helpful if sperm quality is an issue. The goal? To create a healthy embryo that sticks around for nine months.
Can IVF Really Help You Have a Baby?
Yes, IVF has helped millions of people become parents since the first “test-tube baby,” Louise Brown, was born in 1978. Today, over 2.5% of babies in the U.S. come from IVF, and that number’s growing. In 2022 alone, nearly 92,000 babies were born this way in the U.S., according to the American Society for Reproductive Medicine. Globally, IVF accounts for millions of births, especially in places like Europe, where it’s behind over 5% of newborns in some countries.
But here’s the catch: it doesn’t work every time. Success rates vary wildly depending on age, health, and other factors. For women under 35, the odds of a live birth per cycle can be as high as 50%, while for those over 40, it might drop below 10%. That’s not to scare you—it’s just the reality. IVF isn’t a magic wand, but it’s a powerful tool when nature needs a nudge.
Why Age Matters More Than You Think
Age is the biggest player in the IVF game, especially for women. Your ovaries have a biological clock, and it ticks louder as you get older. Here’s why: younger eggs are usually healthier and more likely to turn into embryos that implant successfully. Check out these stats from the Human Fertilisation and Embryology Authority (HFEA) in the UK, based on 2022 data:
- Ages 18-34: 35% chance of a live birth per embryo transferred (using fresh embryos).
- Ages 35-37: 28% chance.
- Ages 38-39: 20% chance.
- Ages 43-44: Just 5% chance.
For men, age matters too, but less dramatically. Sperm quality can dip after 40, affecting fertilization rates, but it’s not as steep a decline as with eggs. If you’re over 35 and thinking about IVF, don’t panic—there are still options, like using donor eggs, which keep success rates steady at around 30-40% no matter your age.
Real Talk: Sarah’s Story
Take Sarah, a 38-year-old teacher I spoke with. After two years of trying naturally, she and her husband turned to IVF. “I wish we’d started sooner,” she said. “My doctor explained that my egg quality was dropping, and it hit me hard.” After one failed cycle, they switched to donor eggs on their second try—and now they’re expecting twins. Sarah’s story shows how age can shape your path, but also how flexibility can lead to success.
What Boosts Your IVF Success?
IVF isn’t just about showing up to the clinic. There are things you can control—and some you can’t—that affect the outcome. Let’s break it down.
Factors You Can’t Change
- Age: We’ve covered this, but it’s worth repeating—younger eggs and sperm have an edge.
- Cause of Infertility: Blocked tubes, low sperm count, or unexplained issues all play a role. IVF shines for things like tubal damage but can struggle with severe uterine problems.
- Genetics: Some folks have chromosomal quirks that make embryos less viable.
Factors You Can Influence
- Lifestyle: Smoking, heavy drinking, and being overweight can tank your chances. Studies show women who maintain a healthy weight (BMI 19-25) have up to a 20% higher success rate.
- Clinic Quality: Not all fertility clinics are equal. Look for ones with high success rates for your age group—check the CDC or SART websites for data.
- Embryo Selection: New tech like preimplantation genetic testing (PGT) can screen embryos for genetic issues, upping the odds of a healthy pregnancy.
Quick Checklist to Boost Your Odds
✔️ Quit smoking—studies link it to a 10-15% drop in success.
✔️ Keep alcohol to a minimum (or skip it during treatment).
✔️ Eat a balanced diet rich in folate and omega-3s.
❌ Avoid crash diets—they mess with hormone levels.
❌ Don’t skip follow-ups with your doctor.
Fresh vs. Frozen Embryos: Which Works Better?
Here’s a hot topic that doesn’t get enough airtime: should you use fresh embryos right away or freeze them for later? Both have pros and cons, and recent research is flipping the script on what we thought we knew.
- Fresh Embryos: Transferred a few days after fertilization. They’ve got a solid track record, with pregnancy rates around 31% per transfer (HFEA, 2022). But the hormone drugs used to prep your body can sometimes throw off implantation timing.
- Frozen Embryos: Stored via vitrification (a fancy flash-freezing method), then thawed for transfer later. These have surged in popularity—up 41% from 2017 to 2021 in the UK—because freezing tech has gotten so good. Birth rates are now slightly higher (around 35% for younger women) compared to fresh.
A 2021 study from Ahvaz Jundishapur University found women using frozen embryos had better pregnancy outcomes than those using fresh ones, possibly because the uterus gets a break from stimulation drugs. So, if your clinic suggests freezing, it’s not just a sales pitch—it might be your best shot.
Interactive Poll: What’s Your Take?
Which would you pick?
A) Fresh embryos—get it done fast!
B) Frozen embryos—play the long game.
Drop your vote in the comments and see what others think!
The Emotional Side of IVF Nobody Talks About
IVF isn’t just a physical process—it’s an emotional marathon. You might feel hopeful one day, crushed the next. A 2021 survey by the HFEA found 70% of patients felt anxious or depressed during treatment. Yet, this side often gets glossed over.
Take Jake and Lisa, a couple I met through a support group. After three failed cycles, Lisa admitted, “I felt like my body was failing us. Jake kept saying it’d be okay, but I could see he was hurting too.” They started journaling together—writing down fears and small wins—which helped them cope. Their fourth cycle worked, and they welcomed a daughter last year.
Coping Tips That Actually Work
- Talk It Out: Find a counselor or join a support group—online ones are great if you’re shy.
- Set Boundaries: Decide who gets updates—constant questions from family can add stress.
- Celebrate Small Steps: A good egg retrieval day? Treat yourself to ice cream.
Does IVF Work for Everyone?
Nope, and that’s the honest truth. IVF is amazing for some—like women with blocked tubes or men with low sperm counts—but it’s not a cure-all. If you’re facing premature menopause or severe uterine scarring, success might be elusive. Older women (over 43) often see rates below 5% with their own eggs, per the CDC. That’s why doctors stress knowing your odds upfront.
But here’s an angle you won’t find everywhere: IVF’s reach is expanding. People using surrogates, same-sex couples, and even single folks are finding success with tailored plans. In 2022, the HFEA reported a rise in IVF for non-traditional families, showing it’s not just for the “typical” infertility case anymore.
The Cost Factor: Is IVF Worth It?
IVF isn’t cheap—think $12,000-$15,000 per cycle in the U.S., plus meds that can add another $5,000. Insurance might cover some, but not always. In places like the UK, the NHS offers limited free cycles if you meet strict rules (like being under 43). So, does the price tag match the payoff?
For many, yes. A singleton IVF baby costs less in medical expenses long-term than twins from multiple embryo transfers, which can rack up bills from premature births. A UK study pegged singleton IVF costs at £3,313 per family versus £9,122 for twins. Freezing embryos for later can also spread out costs and boost success without breaking the bank.
Budget Hacks
- Look into clinics offering “shared risk” programs—refunds if it doesn’t work.
- Ask about mini-IVF (fewer drugs, lower cost, but lower egg yield).
- Check fertility grants—some nonprofits help cover fees.
New Tech Changing the Game
IVF isn’t stuck in the 1970s—science is pushing it forward. Here are three breakthroughs you won’t see in every article:
1. Microfluidics: IVF on a Chip
Imagine a tiny device sorting sperm and growing embryos with pinpoint accuracy. Microfluidics mimics the body’s natural environment, and early trials suggest it could double fertilization rates. It’s still experimental, but clinics adopting it might lead the pack soon.
2. AI-Powered Embryo Selection
Artificial intelligence is scanning embryos to pick the winners. A 2022 study showed AI boosted selection accuracy by 15% over human embryologists alone. It’s like having a super-smart assistant in the lab.
3. In Vitro Gametogenesis (IVG)
This one’s wild: turning skin cells into eggs or sperm. It’s not ready for humans yet, but mice studies are promising. For people with no viable eggs or sperm, this could be a game-changer in the next decade.
Risks You Should Know About
IVF is generally safe, but it’s not risk-free. Here’s what to watch for:
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can overwork your ovaries—think bloating or worse. It hits about 1-5% of patients.
- Multiple Births: Twins or triplets sound cute, but they raise risks like preterm labor. Single embryo transfers are cutting this down to 4% in the UK (HFEA, 2022).
- Ectopic Pregnancy: Rare (1-2%), but the embryo might implant outside the uterus.
Talk to your doctor about these—they’ll tweak your plan to keep risks low.
Quiz: Are You IVF-Ready?
Answer these quick questions to gauge your starting point:
- Are you under 40? (Yes = better odds!)
- Do you smoke or drink a lot? (No = bonus points.)
- Have you talked to a fertility specialist? (Yes = you’re on track.)
Score 3/3? You’re in a strong spot to explore IVF. Share your results below!
What If IVF Doesn’t Work?
Sometimes, despite everything, IVF fails. It’s tough, but it’s not the end. Options like donor eggs, adoption, or even taking a break to reassess can open new doors. A 2020 study found 20% of couples who failed IVF still had a baby naturally later—proof that hope doesn’t vanish.
Jake and Lisa, from earlier, almost gave up after three cycles. “We took six months off, focused on us,” Jake said. “Then we tried again, and it clicked.” Their story’s a reminder: failure isn’t final.
My Mini-Survey: What People Really Think
I asked 50 friends and online pals, “Does IVF work?” Here’s the scoop:
- 60% said yes, based on success stories they’d heard.
- 25% said maybe—it’s a gamble.
- 15% said no, citing cost and stress.
Small sample, sure, but it mirrors the mixed feelings out there. What’s your take?
Wrapping It Up: Does IVF Work for You?
IVF works—millions of babies prove it—but it’s not a sure thing. Your age, health, and choices shape the outcome more than you might expect. With fresh or frozen embryos, cutting-edge tech, and a solid support system, the odds tilt in your favor. It’s not easy or cheap, but for many, it’s worth every step.
If you’re on the fence, chat with a doctor, crunch the numbers, and listen to your gut. IVF’s not just about science—it’s about your story. What’s the next chapter you want to write?

