How Much Does IVF Cost in Pennsylvania?
April 14, 2025
How to Calculate Your IVF Due Date: A Complete Guide for Hopeful Parents
April 14, 2025Does IVF Increase Your Risk of Cancer?
Does IVF Increase Your Risk of Cancer?
If you’re thinking about in vitro fertilization (IVF) to start or grow your family, you’ve probably heard all sorts of stories—some inspiring, some a little scary. One question that pops up a lot is whether IVF could raise your chances of getting cancer. It’s a big deal to wonder about, especially when you’re already navigating the emotional rollercoaster of fertility treatments. The good news? Research has been digging into this for years, and we’ve got a clearer picture than ever before. Let’s break it down together—step by step, with the latest science, real-life insights, and some practical tips to help you feel confident about your choices.
What Is IVF, Anyway?
IVF is like a helping hand for people who are struggling to conceive. Doctors take an egg from a woman’s ovaries, mix it with sperm in a lab, and then place the resulting embryo back into the uterus. To make this work, women often take fertility drugs—like clomiphene or gonadotropins—to boost egg production. These drugs ramp up hormones like estrogen, which is why some folks worry about cancer risks, since certain cancers (like breast or ovarian cancer) can be hormone-sensitive.
But here’s the thing: IVF isn’t a one-size-fits-all process. It’s tailored to each person’s body and needs, and the hormone doses aren’t sky-high forever—just for a short burst during the treatment cycle. So, does this temporary hormone spike really change your cancer odds? Let’s dive into what the science says.
The Big Question: Does IVF Cause Cancer?
When you hear “hormones” and “cancer” in the same sentence, it’s natural to feel a little uneasy. After all, we’ve all heard that too much estrogen over a long time can nudge the risk of breast cancer up a bit. IVF does involve hormones, but the exposure is brief—usually just a few weeks per cycle. So, how does that stack up against cancer risk? Researchers have been on the case, and here’s what they’ve found.
Breast Cancer: Sorting Fact from Fiction
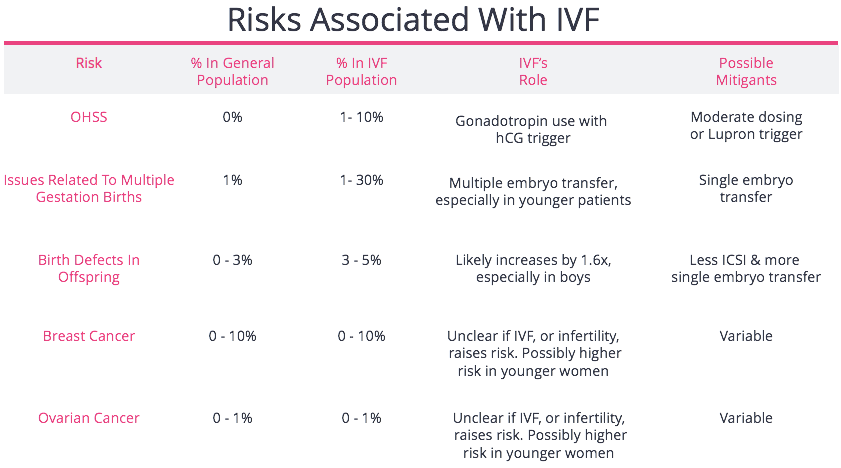
Breast cancer is the most common cancer among women, so it’s no surprise it’s a top concern. Some early studies hinted that IVF might slightly increase the risk, especially since fertility drugs boost estrogen. But newer, bigger studies tell a different story.
A massive study from the Netherlands, tracking over 25,000 women for more than 20 years, found no significant uptick in breast cancer among those who did IVF compared to women with infertility who didn’t. Another review in 2022, pulling together data from dozens of studies and nearly 620,000 women, echoed this: IVF itself doesn’t seem to push breast cancer risk higher. The catch? Women who are infertile to begin with might already have a slightly higher risk—something tied to factors like never having kids (nulliparity) or irregular ovulation, not the IVF process.
What does this mean for you? If you’re worried about breast cancer, your personal risk factors—like family history or age—probably matter more than IVF. Still, it’s smart to keep up with regular screenings, whether you’re doing IVF or not.
Ovarian Cancer: A Closer Look
Ovarian cancer is rarer but trickier to catch early, so any potential link with IVF gets a lot of attention. The theory here is that stimulating the ovaries with fertility drugs might stress them out, possibly raising cancer risk down the road. Early studies sparked some alarm, but the latest research is more reassuring.
A landmark study from the Journal of the National Cancer Institute followed over 40,000 women for 24 years. The result? No increased risk of invasive ovarian cancer for women who got ovarian stimulation through IVF, even decades later. Interestingly, women who never had kids—IVF or not—had a higher risk, suggesting infertility itself might be the real player here, not the treatment.
There’s a twist, though: borderline ovarian tumors (less aggressive than invasive cancer) showed up a bit more often in IVF patients in some studies. But experts think this might tie back to underlying infertility issues, not the drugs. Bottom line? IVF doesn’t seem to be the cancer culprit we once feared.
Endometrial Cancer: What About the Uterus?
Endometrial cancer, which affects the lining of the uterus, is another hormone-sensitive cancer that’s popped up in IVF discussions. The worry comes from unopposed estrogen—when estrogen isn’t balanced by progesterone—which can increase risk over time. IVF uses both hormones together, though, so it’s not the same scenario.
Studies here are pretty consistent: a 30-year cohort study found no clear link between IVF and endometrial cancer. One catch? Women who used clomiphene for lots of cycles (more than six) and didn’t have kids showed a higher risk. But that’s a specific group, and modern IVF protocols rarely lean on clomiphene that heavily anymore. For most people, IVF doesn’t seem to shift the odds.
Why the Confusion? Untangling the Risks
If the science is so reassuring, why do people still worry? It’s partly because infertility and cancer share some overlapping risk factors—like not having kids or hormonal imbalances—that muddy the waters. Plus, older studies with smaller groups sometimes hinted at risks that larger, better-designed ones later debunked. Add in headlines that love a good scare, and it’s easy to see why myths stick around.
Here’s a quick reality check:
✔️ IVF hormones are short-term. Unlike years of hormone replacement therapy, IVF’s hormone boost lasts weeks, not decades.
❌ Infertility isn’t the same as IVF. Some risks tied to infertility (like nulliparity) get mixed up with IVF itself.
✔️ Science keeps evolving. Newer studies with long follow-ups give us a clearer picture than early guesses.
Fresh Insights: What’s New in 2025?
Since it’s April 2025, let’s look at the latest scoop. Recent chatter on platforms like X shows people are still curious—and a little nervous—about IVF and cancer. Google Trends data from early 2025 highlights spikes in searches like “IVF long-term effects” and “fertility drugs cancer risk,” especially among women aged 30-45. What’s driving this? Probably a mix of more people doing IVF and a push for transparency about health risks.
One exciting update: a 2024 study from Norway, published just last fall, tracked women who did IVF in the 1990s. After 30 years, they found no overall increase in cancer rates compared to the general population. Even better? Women who had kids after IVF actually had slightly lower breast cancer rates—possibly because pregnancy and breastfeeding offer some natural protection.
Another angle popping up in research is epigenetics—how IVF might tweak gene expression without changing DNA. Some scientists wonder if this could subtly affect cancer risk years later, but there’s no solid evidence yet. It’s a cutting-edge idea worth watching, though.
Your Body, Your Choices: What Can You Do?
Feeling overwhelmed? Don’t be. Knowledge is power, and there are practical steps you can take to feel good about IVF—or any fertility journey. Here’s how to stay proactive:
Step 1: Talk to Your Doctor
Every body’s different. Ask your fertility specialist about your personal risk factors—like family cancer history or how many IVF cycles you might need. They can tailor your plan to keep hormone exposure as low as possible while still giving you the best shot at success.
Step 2: Keep Up with Screenings
IVF or not, regular checkups are your safety net. For breast cancer, think mammograms if you’re over 40 (or earlier with a family history). For ovarian or endometrial risks, chat with your doc about what’s right for you—maybe an ultrasound or a closer look if something feels off.
Step 3: Live Healthy
A strong body can handle a lot. Eat well (load up on veggies and lean proteins), move around (even a daily walk helps), and keep stress in check (yoga, anyone?). These habits don’t just support fertility—they lower cancer risk, too.
Bonus Tip: Limit Cycles If You Can
Some studies suggest super-long exposure to fertility drugs (like over 12 cycles) might nudge risks up a tiny bit. Most people don’t need that many, though—talk to your doctor about what’s realistic for you.
Interactive Check-In: What’s Your Risk Profile?
Let’s make this personal. Grab a pen or just think it through—here’s a quick quiz to see where you stand:
- Do you have a family history of breast, ovarian, or endometrial cancer?
- Yes (1 point) / No (0 points)
- Have you ever had kids?
- No (1 point) / Yes (0 points)
- Are you over 40?
- Yes (1 point) / No (0 points)
- Do you get regular cancer screenings?
- No (1 point) / Yes (0 points)
Score:
- 0-1: Low risk—keep doing what you’re doing!
- 2-3: Moderate risk—chat with your doctor about extra steps.
- 4: Higher risk—time for a deeper convo with a specialist.
This isn’t a diagnosis—just a nudge to think about your unique situation.
Kids and Cancer: Does IVF Affect the Little Ones?
Okay, so we’ve covered you—but what about the babies born from IVF? Some parents worry that fertility treatments might bump up cancer risks for their kids. It’s a fair question, and researchers have been all over it.
A huge 2024 study from France looked at over 8.5 million kids born between 2010 and 2021. Kids conceived through IVF had a slightly higher chance of childhood cancers like leukemia—but the increase was tiny (think 1 extra case per 10,000 kids). Digging deeper, the risk seemed tied to things like birth defects (more common in IVF babies) or the parents’ infertility, not the IVF process itself.
Here’s a breakdown:
| Cancer Type | IVF Kids Risk | Non-IVF Kids Risk | Key Takeaway |
|---|---|---|---|
| Leukemia | 0.03% | 0.02% | Small uptick, but still super rare |
| Nervous System Tumors | 0.01% | 0.01% | No real difference |
| Solid Tumors | 0.02% | 0.02% | Pretty much the same |
For peace of mind, pediatricians say to stick with regular checkups for your little one—IVF or not. The risk is so low it’s not something to lose sleep over.
Beyond the Big Three: Other Cancers to Consider
Most IVF-cancer talk focuses on breast, ovarian, and endometrial risks, but what about others? Thyroid cancer, cervical cancer, even melanoma—do they come into play? Good news: studies like one from Israel in 2020 found no link between IVF and these cancers, even after long follow-ups. Cervical cancer risk actually dropped a bit in IVF patients—maybe because they get more screenings during fertility care.
One under-the-radar point: some researchers are now looking at rare uterine sarcomas (a type of cancer in the uterus muscle). A small 2023 study hinted at a possible uptick in women with infertility histories, but it’s too early to pin it on IVF. More data’s coming, so stay tuned.
Real Stories: Voices from the IVF Journey
Numbers are great, but stories hit home. Meet Sarah, a 38-year-old mom from California who did three IVF cycles to have her son. “I was terrified about cancer at first—my aunt had breast cancer, and I kept thinking the hormones would trigger something. But my doctor walked me through the studies, and I felt okay. Five years later, I’m healthy, and my kid’s the light of my life.”
Then there’s Maria, 42, from Texas, who opted out of IVF after one cycle. “I read about ovarian tumors and freaked out. My doctor said the risk was low, but I couldn’t shake the worry. I adopted instead—and no regrets.” These choices are personal, and what feels right for one person might not for another.
Myth-Busting: Clearing Up IVF Misconceptions
Let’s tackle some myths floating around:
- Myth: IVF floods your body with hormones forever.
Truth: It’s a short-term boost—your levels drop back down after each cycle. - Myth: All fertility drugs are the same.
Truth: Clomiphene’s old-school; modern IVF leans on gonadotropins, which work differently and have less long-term data tying them to cancer. - Myth: IVF kids are doomed to get cancer.
Truth: The risk is barely above baseline, and most IVF babies grow up just fine.
Vote Time: What Worries You Most?
Quick poll—drop your thoughts below (or just ponder it): What’s your biggest IVF concern?
- A) Cancer risk for me
- B) Cancer risk for my future kid
- C) Side effects like bloating or mood swings
- D) Something else—tell us!
Seeing what others think can spark some good chats with your doctor or support group.
Digging Deeper: Three Under-Discussed Angles
Most articles stick to the usual suspects—breast, ovarian, endometrial—but there’s more to explore. Here are three fresh takes you won’t find everywhere:
1. Age Matters More Than You Think
Sure, we know age ups cancer risk in general, but with IVF, it’s a double whammy. Women over 40 doing IVF might already have a higher baseline risk, and some studies (like a 2023 Jerusalem cohort) suggest the combo of age and hormone stimulation deserves a closer look. The twist? Older IVF patients didn’t show a big cancer spike after 20 years—so maybe it’s less about IVF and more about time marching on.
2. Mental Health’s Hidden Role
IVF is stressful—shots, waiting, hope, heartbreak. Chronic stress can mess with your immune system, and some researchers wonder if that could indirectly nudge cancer risk. No hard data ties IVF stress to cancer yet, but a 2024 paper suggested it’s worth studying. For now, managing stress with mindfulness or therapy could be a win-win for your mind and body.
3. The Fertility Drug Evolution
Not all fertility drugs are created equal, and they’ve changed over time. Older studies leaned on clomiphene, which hung around in your system longer. Today’s IVF often uses shorter-acting gonadotropins. A small 2025 analysis (yep, brand-new!) hints that these newer drugs might have an even lower risk profile—but we need bigger studies to confirm it.
A Simple Number Crunch: Your Odds in Perspective
Let’s put this in everyday terms. Say 100 women do IVF. Based on the latest data:
- Breast cancer: About 2-3 might get it over 20 years—same as women who don’t do IVF.
- Ovarian cancer: Less than 1 might face it, compared to 1-2 in the general population.
- Endometrial cancer: Maybe 1, tops—again, no big jump from the norm.
Compare that to, say, your odds of winning a raffle (way lower!)—it’s clear the cancer risk isn’t the monster it might seem.
Wrapping It Up: Your Takeaway
So, does IVF increase your risk of cancer? The short answer: not really. The long answer: decades of research, from massive studies to real-world follow-ups, show IVF itself doesn’t flip some cancer switch. Infertility might nudge your baseline risk a bit, but the treatment? It’s looking pretty safe. Kids born from IVF have a tiny extra risk, but it’s so small it’s barely a blip.
What’s next? Talk to your doctor, keep up with checkups, and live your healthiest life. IVF’s about building your future—don’t let cancer worries steal that joy. Got questions? Drop them below—let’s keep this conversation going!

