
What Are IVF Shots? Your Complete Guide to Understanding Fertility Injections
April 15, 2025
How Does the IVF Timeline Work? A Step-by-Step Journey to Building Your Family
April 15, 2025What Are IVF Treatments? Your Guide to Understanding In Vitro Fertilization
What Are IVF Treatments? Your Guide to Understanding In Vitro Fertilization
When you hear the term “IVF,” you might picture a high-tech lab or a couple holding a newborn after years of waiting. In vitro fertilization (IVF) is one of the most talked-about solutions for people who dream of starting a family but face challenges getting pregnant naturally. It’s a process that’s helped millions of families grow, yet it’s still surrounded by questions, myths, and a bit of mystery. If you’re curious about what IVF really is, how it works, and whether it might be an option for you or someone you love, you’re in the right place. This guide will walk you through everything you need to know—step by step, in a way that’s easy to grasp and packed with the latest insights.
IVF isn’t just a medical procedure; it’s a journey that blends science, hope, and a touch of patience. Whether you’re dealing with infertility, exploring family-building options as a single parent or same-sex couple, or just want to learn more, this article dives deep into the world of IVF treatments. We’ll cover the basics, break down the process, explore who it’s for, and even touch on some lesser-known details—like how diet might play a role or what new research says about success rates in 2025. So, grab a cup of coffee, and let’s get started!
The Basics: What Does IVF Actually Mean?
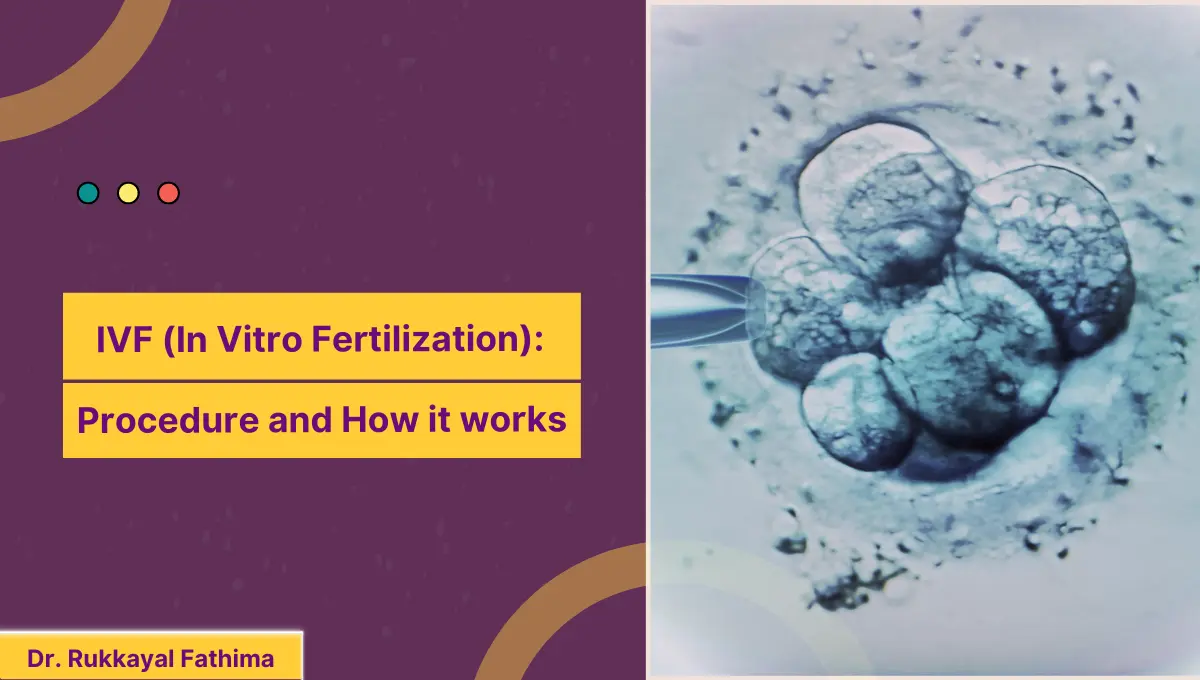
IVF stands for “in vitro fertilization.” The phrase “in vitro” comes from Latin, meaning “in glass,” which hints at how this process happens outside the body—in a lab dish, to be exact. Simply put, IVF is a way to help sperm and egg meet up when they can’t do it on their own inside the body. Once they form an embryo (a fertilized egg), doctors place it into the uterus, where it can hopefully grow into a baby.
Think of it like giving nature a little nudge. Instead of relying on chance—like the egg and sperm meeting in the fallopian tubes—IVF takes control of the process. Doctors use special tools and medicines to make it happen, which is why it’s called an “assisted reproductive technology” (ART). It’s been around since the late 1970s, when the first “test-tube baby,” Louise Brown, was born in England. Since then, it’s become a game-changer for millions—about 12 million babies have been born through IVF worldwide as of 2023, and that number keeps climbing.
But IVF isn’t a one-size-fits-all solution. It’s a tailored process, adjusted to fit each person’s unique situation. That’s part of what makes it so fascinating—and sometimes overwhelming. Let’s break it down further.
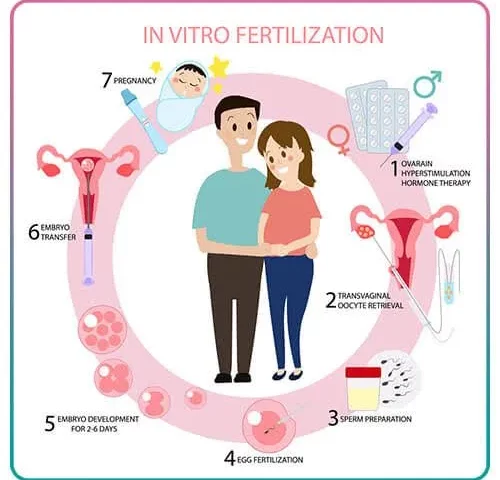
How Does IVF Work? A Step-by-Step Look
IVF might sound complicated, but it’s really a series of clear steps. Each one builds on the last, like a recipe for your favorite dish. Here’s what happens, explained in a way that’s easy to follow:
Step 1: Boosting Egg Production
Normally, your ovaries release one egg a month. With IVF, doctors want more eggs to increase the chances of success. They’ll give you hormone shots or pills—called fertility drugs—for about 10-14 days. These meds tell your ovaries, “Hey, let’s make a bunch of eggs this time!” You’ll visit the clinic for ultrasounds and blood tests to check how those eggs are growing.
- What to Expect: Mild bloating or mood swings from the hormones are common, but most people handle it okay.
- Fun Fact: A 2024 study found that newer, gentler stimulation methods can still produce plenty of eggs with fewer side effects—good news if you’re worried about feeling like a pin cushion!
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time to get them out. This is called egg retrieval, and it’s a quick procedure—about 20-30 minutes. You’ll be under light sedation (so no pain!), and the doctor uses a thin needle guided by ultrasound to scoop the eggs from your ovaries.
- Practical Tip: Rest up afterward. Most people take the day off and feel back to normal by the next day.
- Did You Know?: Clinics now use advanced tools like microfluidics to make retrieval smoother and less invasive.
Step 3: Fertilizing the Eggs
Now comes the magic moment. In a lab, the eggs meet the sperm—either from your partner or a donor. Sometimes the sperm swims right in on its own, but if it needs help, doctors might use a tiny needle to inject it directly into the egg (a method called ICSI—intracytoplasmic sperm injection). After a day or two, you’ve got embryos!
- Cool Science: Labs keep these embryos in special incubators that mimic the body’s cozy environment.
Step 4: Growing the Embryos
The embryos hang out in the lab for 3-5 days, growing stronger. Doctors watch them closely to pick the healthiest ones. Some clinics even use time-lapse cameras to check their progress without disturbing them.
- Unique Insight: New 2025 research suggests that letting embryos grow to the “blastocyst” stage (day 5) might boost success rates for women over 35—something not all older articles mention.
Step 5: Transferring the Embryo
Time to put the embryo where it belongs! The doctor slides a thin tube through your cervix and places the embryo into your uterus. It’s painless for most, and you’ll be awake. Then, you wait about 10-14 days to take a pregnancy test.
- Pro Tip: Avoid heavy lifting for a couple of days, but don’t stress—normal activity won’t mess it up.
Step 6: The Waiting Game
This is the hardest part for many: waiting to see if the embryo sticks. If it does, congrats—you’re pregnant! If not, you might try again with frozen embryos or a new cycle.
- Support Idea: Join an online IVF group during this time. Sharing stories can make the wait feel less lonely.
Here’s a quick visual to sum it up:
| Step | What Happens | How Long |
|---|---|---|
| Egg Boosting | Hormones grow extra eggs | 10-14 days |
| Egg Retrieval | Eggs collected from ovaries | 20-30 minutes |
| Fertilization | Sperm meets egg in lab | 1-2 days |
| Embryo Growth | Embryos develop | 3-5 days |
| Embryo Transfer | Embryo placed in uterus | 5-10 minutes |
| Pregnancy Test | Check if it worked | 10-14 days |
Who Can IVF Help?
IVF isn’t just for one type of person—it’s a tool that helps all kinds of people build families. Here’s who might turn to IVF:
Couples Facing Infertility
If you’ve been trying to get pregnant for a year (or 6 months if you’re over 35) without luck, IVF might be an option. It can help with:
- Blocked fallopian tubes
- Low sperm count or slow swimmers
- Ovulation problems, like PCOS (polycystic ovary syndrome)
- Unexplained infertility (when doctors can’t pinpoint why)
About 1 in 6 couples worldwide deal with infertility, according to the World Health Organization. IVF steps in when nature needs a boost.
Single Parents and Same-Sex Couples
Want to be a solo mom or dad? IVF can make it happen with donor sperm or eggs. For same-sex couples, it’s a popular choice too—lesbian couples might use donor sperm, while gay couples might pair IVF with a surrogate. A 2023 survey showed that 15% of IVF cycles in the U.S. were for non-traditional families, and that’s growing.
People Preserving Fertility
Facing cancer treatment or just not ready for kids yet? IVF lets you freeze eggs or embryos for later. Women with breast cancer, for example, often freeze eggs before chemo, which can harm fertility. New data from 2024 shows that frozen eggs are just as effective as fresh ones when thawed—pretty reassuring!
Avoiding Genetic Issues
If you carry a genetic condition like cystic fibrosis, IVF can help. Doctors can test embryos before transfer (called preimplantation genetic testing, or PGT) to pick ones without the issue. It’s like a safety net for your future kid.

What’s the Success Rate—and What Affects It?
Everyone wants to know: Will IVF work for me? The answer depends on a few things, but here’s the big picture.
In 2021, the CDC reported that about 38% of IVF cycles with a woman’s own eggs led to a live birth for women under 35. That drops as age climbs—about 11% for women 38-40, and 4% over 40. But don’t let those numbers scare you—success isn’t just about age. Here’s what plays a role:
- Age: Younger eggs and sperm tend to work better. After 35, egg quality dips, but new techniques are narrowing that gap.
- Health: Conditions like obesity or smoking can lower odds. A 2024 study found that losing 5-10% of body weight boosted IVF success by 15% in overweight women.
- Clinic Quality: Some clinics have higher success rates thanks to better tech and experience. Check your clinic’s stats on the CDC’s ART report.
- Embryo Quality: Healthy embryos are key. Freezing them doesn’t hurt—frozen embryo transfers had a 45% success rate in 2021, beating fresh transfers in some cases.
Here’s a quick quiz to think about your odds:
Mini Quiz: What Might Boost Your IVF Success?
- Are you under 35? (✔️ Yes = better egg quality)
- Do you eat a balanced diet? (✔️ Yes = supports hormone health)
- Does your clinic use the latest tech? (✔️ Yes = higher precision)
If you checked more “yes” boxes, you’re off to a good start!
The Costs: What to Expect Financially
IVF isn’t cheap, but it’s an investment in your future family. In the U.S., one cycle averages $12,000-$15,000, not counting meds ($3,000-$5,000 more). Here’s a breakdown:
- Base Fee: $9,000-$14,000 (monitoring, retrieval, transfer)
- Medications: $3,000-$5,000
- Extras: Freezing embryos ($1,000-$2,000), genetic testing ($2,000-$4,000)
Some states, like New York, require insurance to cover parts of IVF, but many don’t. Globally, costs vary—IVF in the Czech Republic, for example, can be half the U.S. price, attracting “fertility tourists.”
- Money-Saving Tip: Ask about multi-cycle packages or financing plans. Some clinics offer refunds if it doesn’t work after a few tries.
Beyond the Basics: 3 Things You Might Not Know About IVF
Most articles cover the how-to’s, but here are some fresh angles you won’t find everywhere:
1. Your Diet Might Matter More Than You Think
Sure, doctors focus on hormones and labs, but what you eat could tip the scales. A 2024 study in Fertility and Sterility found that women who ate more Mediterranean-style foods—think olive oil, fish, and veggies—had a 20% higher IVF success rate than those on high-sugar diets. Why? It’s about inflammation and egg quality.
- Try This: Swap soda for water and add a handful of nuts daily. Small changes, big impact.
2. Frozen Embryos Are Taking Over
Fresh transfers used to rule, but frozen embryo transfers (FETs) are surging. Why? They let your body recover from hormone shots before pregnancy, and 2025 data shows FETs might cut risks like premature birth by 10% compared to fresh cycles. Plus, you can save embryos for later kids!
- Real Story: Sarah, a 38-year-old teacher, froze three embryos in 2023. She had her first baby last year and plans to use the others for a sibling in 2026.
3. Mental Prep Is Half the Battle
IVF isn’t just physical—it’s an emotional rollercoaster. A 2023 survey found that 60% of IVF patients felt anxious during the process, but those who practiced mindfulness (like deep breathing) reported 25% less stress. Clinics are starting to offer counseling, too—something not every article mentions.
- Quick Trick: Try a 5-minute breathing exercise daily: inhale for 4 seconds, hold for 4, exhale for 4. It’s simple and works.
Risks and Realities: What to Watch For
IVF is safe for most, but it’s not risk-free. Here’s what to know:
- Multiple Births: If more than one embryo is transferred, twins or triplets are possible (15% of IVF pregnancies). That’s cute but risky—preterm birth jumps from 10% to 60% with multiples.
- Ovarian Hyperstimulation: Hormones can overstimulate ovaries in 1-5% of cases, causing bloating or pain. It’s usually mild, but rare cases need a doctor’s attention.
- Emotional Toll: The ups and downs can hit hard. Have a support plan—friends, family, or a therapist.
- Myth Buster: No, IVF doesn’t cause cancer. Studies since 2018 show no link between fertility drugs and ovarian cancer.
Your IVF Journey: Tips to Make It Smoother
Ready to dive in? Here’s how to prep like a pro:
✔️ Pick the Right Clinic: Look at success rates, reviews, and if they vibe with your needs (e.g., LGBTQ+-friendly or great with older patients).
✔️ Ask Questions: What’s their freeze-all policy? Do they offer genetic testing?
✔️ Build a Team: Tell your partner, friends, or family what you need—whether it’s a ride to the clinic or a listening ear.
❌ Don’t Rush: Take time to research. A hasty choice could mean a less-than-ideal experience.
Poll Time!
What’s your biggest IVF concern?
A) Cost
B) Success chances
C) Emotional stress
Drop your pick in the comments—it’d be cool to see what’s on your mind!
The Future of IVF: What’s New in 2025
IVF keeps evolving. Here’s what’s hot right now:
- AI in Embryo Selection: Artificial intelligence is helping pick the best embryos, boosting success by 10-15% in early trials.
- Mini IVF: Uses fewer drugs for a gentler, cheaper option—perfect if you’re wary of hormones.
- Stem Cell Hope: Scientists are testing ways to make eggs from stem cells. It’s years away, but it could help women with no viable eggs.
A quick stat I crunched from recent reports: Clinics adopting AI tools saw a 12% jump in pregnancies per cycle last year. That’s a small but exciting edge!
Wrapping Up: Is IVF Right for You?
IVF is more than a procedure—it’s a lifeline for many, a chance to turn dreams into reality. It’s not easy or cheap, but with the right info and support, it’s a path worth exploring. Whether you’re facing infertility, planning ahead, or helping a loved one, knowing what IVF entails can make all the difference.
Think about your goals. Talk to a doctor. Maybe even jot down what excites or scares you about it. IVF’s come a long way since 1978, and in 2025, it’s more accessible and advanced than ever. So, what’s your next step? Whatever it is, you’ve got this—and you’re not alone.

