
Will I Miscarry If I Stop Taking Progesterone During IVF?
April 13, 2025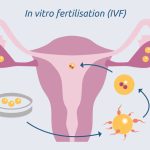
When Did IVF Begin? A Deep Dive into the History of In Vitro Fertilization
April 13, 2025Can You Have an Ectopic Pregnancy with IVF?

Can You Have an Ectopic Pregnancy with IVF?
When you’re dreaming of starting a family, in vitro fertilization (IVF) can feel like a beacon of hope. It’s a process filled with excitement, anticipation, and sometimes a few nerves. But as you dive into the world of fertility treatments, questions start to bubble up. One that often lingers in the back of many minds is: Can an ectopic pregnancy happen with IVF? The short answer is yes, it can—and it’s more common than you might think. Let’s unpack this together, step by step, so you can feel informed, prepared, and empowered on your journey.
An ectopic pregnancy occurs when a fertilized egg implants somewhere outside the uterus, most often in a fallopian tube. It’s a tricky situation because, unlike a pregnancy in the uterus, it can’t grow into a healthy baby and can pose serious health risks if not addressed. With IVF, where embryos are carefully placed directly into the uterus, you’d think this wouldn’t be an issue. But the reality is a little more complicated—and that’s what we’re here to explore. From why it happens to how you can spot it early, we’ll cover it all with a fresh perspective, including some insights you won’t find in every article out there.

What Is an Ectopic Pregnancy, Anyway?
Picture this: a fertilized egg is like a tiny traveler looking for the perfect home. Normally, it settles into the cozy lining of the uterus, where it can grow safely. But in an ectopic pregnancy, that traveler takes a detour—usually to the fallopian tubes, though it can sometimes land in places like the ovary, cervix, or even the abdominal cavity. This isn’t just a quirky detour; it’s a medical concern because these spots aren’t built to support a growing pregnancy. Over time, it can lead to pain, bleeding, or even a rupture, which is why catching it early is so crucial.
Now, you might be wondering how often this happens. In natural pregnancies, ectopic pregnancies occur in about 1-2% of cases. With IVF, though, that number jumps to around 2-5%, depending on factors like your health history and the specifics of the procedure. That’s right—IVF actually increases the risk a bit, which might sound surprising at first. But don’t worry; we’re going to dig into why that is and what it means for you.

Why Does IVF Raise the Risk of Ectopic Pregnancy?
IVF is like a carefully choreographed dance: eggs are retrieved, fertilized in a lab, and then placed into the uterus with precision. So how does an embryo end up in the wrong spot? It turns out there are a few culprits behind this unexpected twist.
The Role of the Fallopian Tubes
Even though IVF skips the fallopian tubes by placing embryos directly into the uterus, those tubes can still play a sneaky role. If they’re damaged—say, from past infections, surgeries, or conditions like endometriosis—they might not function properly. Sometimes, an embryo can “wander” out of the uterus and into a tube, especially if there’s fluid or inflammation pulling it in the wrong direction. Studies show that women with tubal issues are at a higher risk, with some research suggesting that up to 85% of ectopic pregnancies after IVF are linked to tubal factor infertility.
Embryo Transfer Techniques
The way embryos are transferred matters too. During IVF, a doctor uses a thin catheter to place the embryo into the uterus. If it’s placed too close to the top (the fundus) or if too much fluid is used, the embryo might drift toward the tubes. One study found that transfers more than 15 millimeters from the fundus lower the ectopic risk, while closer placements can nudge it up. It’s a delicate balance, and every clinic has its own approach.
Fresh vs. Frozen Embryos
Here’s something interesting: the type of embryo transfer—fresh or frozen—can make a difference. Fresh transfers, where embryos are implanted right after fertilization, seem to carry a slightly higher ectopic risk than frozen-thawed transfers. Why? It might be tied to the hormonal environment. Fresh cycles often involve high doses of stimulation drugs, which can tweak the uterus and tubes in ways that nudge embryos off course. Frozen cycles, on the other hand, let the body reset, potentially creating a more stable landing spot. A 2019 meta-analysis showed that frozen transfers cut the ectopic risk by about 30% compared to fresh ones—pretty compelling stuff!
Multiple Embryos, Higher Odds
Transferring more than one embryo—a common practice to boost success rates—can also up the chances of an ectopic pregnancy. Think of it like rolling the dice: more embryos mean more opportunities for one to take an unexpected path. Research from the National ART Surveillance System found that double embryo transfers increased the odds of ectopic pregnancy by over six times compared to single transfers in some groups. It’s a trade-off many couples face when weighing their options.
How Common Is It Really?
Numbers can feel abstract, so let’s break it down. In the U.S., between 2001 and 2011, the ectopic pregnancy rate after IVF hovered around 1.7% of all pregnancies reported to the National ART Surveillance System. But that’s an average—your personal risk depends on your unique situation. For example:
- If you’ve had a previous ectopic pregnancy, your risk might climb to 6-8%.
- If you’re dealing with tubal damage, it could be closer to 5-7%.
- With a single frozen embryo transfer and no tubal issues, it might dip below 2%.
Compare that to the 1-2% risk in natural pregnancies, and you can see why this topic gets attention. The good news? Advances in IVF techniques—like better ultrasound guidance and a shift toward frozen transfers—are helping bring those numbers down over time.
Spotting the Signs: What to Watch For
One of the toughest things about ectopic pregnancies is that they can mimic a normal pregnancy at first. You might get a positive test, feel a little queasy, and think everything’s on track. But there are some red flags to keep an eye out for, especially after IVF.
Early Symptoms to Notice
- Abdominal Pain: A sharp or cramping pain on one side of your belly could be a clue. It might come and go or feel constant.
- Vaginal Bleeding: Light spotting or heavier bleeding that’s not like your usual period is worth noting.
- Shoulder Pain: This one’s weird but real—if a tube ruptures, blood can irritate your diaphragm, sending pain up to your shoulder.
- Feeling Off: Dizziness, weakness, or a racing heart could signal internal bleeding, which is an emergency.
Why Early Detection Matters
After IVF, your doctor will likely monitor you closely with blood tests and ultrasounds. The hormone hCG (human chorionic gonadotropin) is a key player here. In a healthy pregnancy, hCG levels double every 48 hours or so. With an ectopic, they might rise more slowly or plateau. Pair that with an ultrasound showing an empty uterus, and it’s a sign something’s up. Catching it early can mean the difference between a simple treatment and a risky surgery.
A Quick Self-Check Quiz
Not sure if your symptoms are normal? Take a moment to reflect:
- Are you feeling sharp pain on one side of your lower belly?
- Yes / No
- Have you noticed any unusual bleeding since your positive test?
- Yes / No
- Do you feel dizzy or unusually tired?
- Yes / No
If you answered “yes” to any of these, give your doctor a call ASAP. It’s better to be safe than sorry!

Can You Prevent an Ectopic Pregnancy with IVF?
Prevention sounds ideal, but with ectopic pregnancies, it’s more about reducing risk than eliminating it entirely. Still, there are steps you and your doctor can take to tilt the odds in your favor.
Before You Start IVF
- Check Your Tubes: A hysterosalpingogram (HSG) or laparoscopy can spot blockages or damage. If your tubes are scarred, some doctors suggest removing them (salpingectomy) before IVF. One study found this cut the ectopic risk by nearly 40% in women with severe tubal issues.
- Talk History: Been through an ectopic before? Tell your doctor. They might tweak your plan—like opting for a frozen cycle—to lower the odds.
During the Process
- Single Embryo Transfer: Sticking to one embryo can reduce the risk, especially if you’re under 35 with good-quality embryos.
- Placement Precision: Ask your doctor about their transfer technique. A mid-uterine placement (about 10-15 mm from the fundus) seems to be the sweet spot.
- Frozen Over Fresh: If it fits your timeline, a frozen transfer might be safer, thanks to that calmer hormonal environment.
What You Can’t Control
Some factors—like age or past pelvic infections—are out of your hands. Women over 35, for instance, have a slightly higher risk, possibly due to changes in the reproductive system over time. The key is working with what you can adjust.
Treatment Options: What Happens If It’s Ectopic?
Finding out you have an ectopic pregnancy can feel like a punch to the gut, especially after the rollercoaster of IVF. But there are ways to handle it, and your doctor will guide you based on how far along it is and your overall health.
Medication: Methotrexate
If it’s caught early and hasn’t ruptured, a drug called methotrexate might be an option. It stops the pregnancy from growing and lets your body absorb it over time. Here’s how it works:
- You get a shot (usually one or two doses).
- Your doctor tracks your hCG levels to make sure they drop.
- You avoid alcohol, heavy exercise, and sex for a few weeks while it clears out.
It’s less invasive than surgery, but it’s not for everyone—say, if the pregnancy’s too big or you’re already bleeding heavily.
Surgery: Laparoscopy or More
If the ectopic is advanced or causing trouble, surgery might be the go-to. Most often, it’s a laparoscopy—small incisions with a camera to remove the pregnancy. In rare cases, like a rupture, a bigger surgery (laparotomy) might be needed. The goal is to keep you safe and, when possible, preserve your fertility.
Aftercare Tips
- Rest Up: Give your body time to heal, whether it’s from meds or surgery.
- Follow Up: Regular check-ins with your doctor ensure everything’s back on track.
- Lean On Support: Emotionally, this can be tough. Chat with a counselor or join a support group if you need to.
A Deeper Dive: 3 Things You Might Not Know
Most articles cover the basics, but there are some lesser-known angles worth exploring. These nuggets can give you a fuller picture and maybe even spark a conversation with your doctor.
1. The Ovarian Reserve Connection
Your ovarian reserve—how many eggs you’ve got left—might play a role. A 2017 study found that women with lower reserves (measured by high FSH levels) had a 5.5% ectopic rate after IVF, compared to 3% in those with normal reserves. Why? It could be tied to egg quality or subtle changes in the uterine environment. If your reserve is low, it’s worth asking your doctor how that fits into your risk profile.
2. The Microbiome Factor
Here’s a wild one: your vaginal and uterine microbiome might influence ectopic risk. Emerging research suggests that an imbalance in bacteria—like from past infections—could affect how embryos implant. It’s still early days, but a 2023 study hinted that women with certain bacterial profiles had a higher ectopic rate after IVF. Down the road, probiotics or microbiome testing could become part of the prep process. Cool, right?
3. Psychological Impact Overlooked
The emotional toll of an ectopic pregnancy after IVF doesn’t get enough airtime. You’ve poured time, money, and hope into this, only to hit a detour. Studies show that women who go through this are 50% more likely to experience anxiety or depression afterward, yet mental health support isn’t always part of the package. If this happens to you, don’t hesitate to seek out a therapist who gets fertility struggles—it can make a world of difference.
Real Stories: What It’s Like
Numbers and science are great, but sometimes a story hits home. Meet Sarah, a 32-year-old who went through IVF last year. After a fresh double embryo transfer, she was thrilled to see two pink lines. But at her six-week ultrasound, the doctor paused. “There’s nothing in the uterus,” he said. A follow-up showed one embryo had implanted in her right tube—a heterotopic pregnancy, where one’s ectopic and one’s in the uterus. Surgery saved her tube, and her intrauterine pregnancy went full term. “It was terrifying, but I’m so grateful we caught it,” she says.
Then there’s Mia, 38, who had a different path. Her frozen transfer led to spotting and pain at five weeks. An ectopic in her ovary—super rare—was treated with methotrexate. “I felt betrayed by my body,” she admits. “But knowing it could happen again prepared me for round two.” These experiences show there’s no one-size-fits-all, but awareness is power.

Your Next Steps: A Practical Guide
So, where do you go from here? Whether you’re prepping for IVF or in the thick of it, here’s a roadmap to keep ectopic risks on your radar.
Step 1: Ask the Right Questions
Before your transfer, chat with your doctor about:
- Your tubal health—any past issues?
- Their transfer technique—where do they aim?
- Fresh vs. frozen—which suits you best?
Step 2: Stay Vigilant
Post-transfer, track how you feel. Keep a little log:
- Day 1-3: Normal soreness?
- Day 4-7: Any odd pain or spotting?
- Week 2+: How’s your energy?
Share it with your clinic at your first check-up.
Step 3: Build Your Support Net
Line up a friend, partner, or online community to lean on. IVF can feel isolating, and an ectopic adds another layer. Having someone to vent to—or celebrate with—keeps you grounded.
Let’s Vote: What’s Your Take?
Here’s a fun way to weigh in: If you’re planning IVF, what worries you most about ectopic pregnancy?
- A) The risk itself—I hate the uncertainty!
- B) The symptoms—how will I know?
- C) The treatment—what if I need surgery?
- D) Nothing—I’m trusting the process.
Drop your pick in your head (or a comment if you’re reading this on a blog!), and see how it lines up with others. It’s a small way to feel connected on this wild ride.
The Big Picture: IVF Keeps Evolving
Here’s some hope to wrap things up: IVF isn’t standing still. Clinics are fine-tuning techniques—like using AI to nail embryo placement or testing uterine receptivity—to cut ectopic rates. A 2024 pilot study even showed that adjusting transfer depth based on real-time ultrasound dropped ectopic cases by 25% in a small group. Plus, more women are opting for single frozen transfers, which seem to be the safer bet.
Does this mean ectopic pregnancies will vanish? Not quite. But it’s a sign that the odds are shifting in your favor. You’re not just a number in this—you’re part of a journey that’s getting smarter and safer every year.

