What Does IVF Do?
April 12, 2025
What Is IVF? Your Complete Guide to In Vitro Fertilization
April 12, 2025What Is the Process of IVF?
What Is the Process of IVF?
If you’ve ever wondered how a tiny spark of life can begin outside the body and grow into a baby, you’re not alone. In vitro fertilization, or IVF, is a fascinating journey that’s helped millions of people build families when nature needs a little nudge. It’s not just a medical procedure—it’s a mix of science, hope, and a lot of patience. Whether you’re curious about it for yourself, a loved one, or just because it’s cool to know, this guide will walk you through every step of the process. We’ll break it down into bite-sized pieces, sprinkle in some real-world insights, and even throw in a few surprises that you won’t find in the usual rundown. Ready? Let’s dive in.
The Big Picture: What IVF Really Is
IVF is like a backstage pass to conception. Normally, a baby starts when an egg and sperm meet inside a woman’s body. But with IVF, that meeting happens in a lab—specifically, in a petri dish (yep, “in vitro” literally means “in glass” in Latin). After the egg is fertilized and grows into an embryo, it’s carefully placed back into the uterus to hopefully become a pregnancy. It’s a process that’s been around since 1978, when the first IVF baby, Louise Brown, was born in England. Since then, over 8 million babies have come into the world this way.
Why do people turn to IVF? Sometimes it’s because of blocked fallopian tubes, low sperm count, or conditions like endometriosis. Other times, it’s for same-sex couples, single parents-to-be, or folks wanting to avoid passing on genetic issues. Whatever the reason, IVF is a lifeline—a chance to make dreams come true when the usual path isn’t working.
Step 1: Getting the Ovaries Ready
The IVF journey starts with a boost to the ovaries. In a natural cycle, your body usually releases just one egg a month. But IVF likes to stack the odds, so doctors use fertility drugs to encourage your ovaries to produce multiple eggs. Think of it like turning up the volume on a quiet song—suddenly, there’s a whole chorus of eggs ready to join the party.
How It Works
For about 8 to 14 days, you’ll take medications—usually shots you give yourself at home. These drugs, called gonadotropins, tell your ovaries to get busy. Your doctor will keep a close eye on things with blood tests and ultrasounds, tracking how many egg-containing sacs (follicles) are growing and how big they’re getting. When the follicles hit the right size—around 14 to 20 millimeters—it’s almost go-time.
What to Expect
- ✔️ Daily Check-ins: You might visit the clinic a few times for monitoring.
- ❌ No Skipping Doses: Missing a shot can throw off the whole plan.
- ✔️ Teamwork: Nurses often teach you how to inject yourself—don’t worry, it’s easier than it sounds!
A Little Science
Studies show that women under 35 can produce an average of 10-15 eggs per cycle with these meds, according to the CDC’s 2022 fertility data. More eggs mean more chances for a healthy embryo, but it’s not a guarantee. Quality matters just as much as quantity.
Pro Tip
Start a mini journal to track how you feel each day. Some folks breeze through this phase, while others feel bloated or emotional from the hormones. Knowing what’s normal for you can ease the stress.
Step 2: Triggering the Release
Once your eggs are ready, it’s time to give them the green light to mature fully. This step is all about timing—too early or too late, and the eggs won’t be in prime shape. Your doctor uses a “trigger shot” to make this happen, usually a dose of human chorionic gonadotropin (hCG), which mimics the hormone that naturally sparks ovulation.
The Timing Game
About 36 hours after the trigger shot, your eggs will be ripe for picking. The catch? They need to be collected before they pop out on their own, so the retrieval is scheduled like clockwork—usually 34 to 36 hours post-shot.
Fun Fact
Ever wonder why it’s 36 hours? Research from the American Society for Reproductive Medicine (ASRM) shows that’s the sweet spot when eggs are mature but still snug in their follicles, making them easier to grab.
Quick Checklist
- ✔️ Rest up the night before—retrieval day is coming!
- ❌ No food or drink after midnight before the procedure (your clinic will confirm).
- ✔️ Ask about pain relief options if you’re nervous.
This step feels like the calm before the storm—it’s quiet, but the excitement (and maybe some nerves) is building.
Step 3: Egg Retrieval—Harvest Time!
Now comes the big moment: collecting those eggs. This is a short procedure, about 15-20 minutes, done under light anesthesia so you’re comfy and snoozing. The doctor uses a thin needle guided by ultrasound to gently pull the eggs from your ovaries.
What Happens
Picture this: a tiny vacuum cleaner sucks the eggs and some fluid out of each follicle through the needle. The fluid goes straight to the lab, where an embryologist hunts for the eggs under a microscope. On average, 10-15 eggs are collected, though it varies.
Real Talk
It’s normal to feel crampy or sore afterward—think mild period vibes. Most people are back to light activities the next day. One woman I heard about described it as “like a weird science field trip—I didn’t feel a thing, but I was fascinated later!”
Science Spotlight
A 2023 study in Fertility and Sterility found that retrieving 10+ eggs ups the odds of a successful IVF cycle by 20% for women under 38. But more isn’t always better—too many can lead to a rare condition called ovarian hyperstimulation syndrome (OHSS). Luckily, it affects less than 5% of patients.
Your Move
- ✔️ Bring a buddy to drive you home—you’ll be groggy.
- ❌ Don’t panic if you spot a little blood; it’s common.
- ✔️ Stock up on cozy socks and a heating pad for recovery.
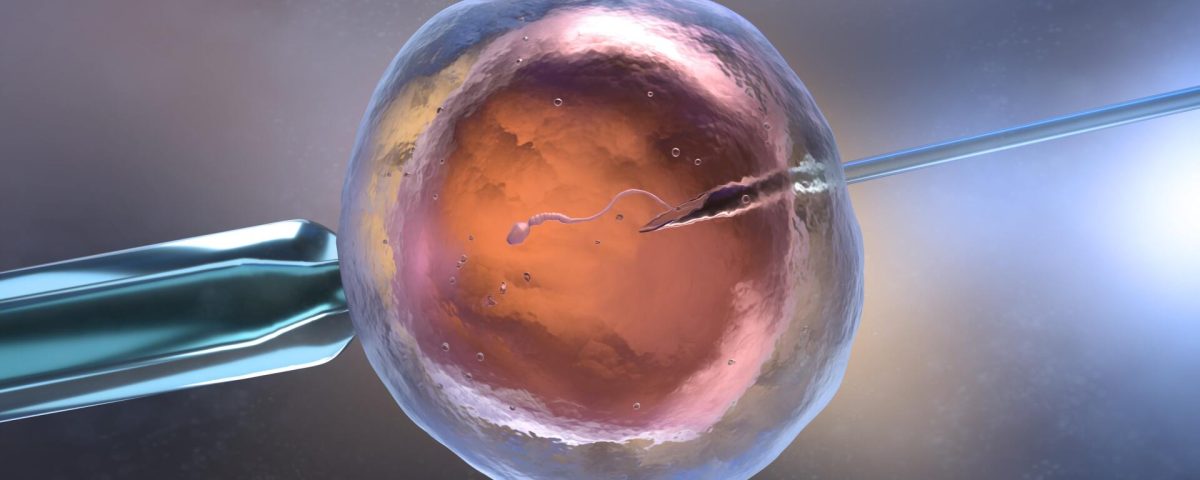
Step 4: Sperm Meets Egg in the Lab
While you’re resting, the real magic happens in the lab. The embryologist pairs your eggs with sperm—either from a partner or a donor. There are two ways this can go: traditional IVF, where sperm and eggs mingle in a dish, or intracytoplasmic sperm injection (ICSI), where a single sperm is injected right into an egg.
The Fertilization Dance
- Traditional IVF: Thousands of sperm swim around each egg, hoping one gets through. It’s like a mini competition.
- ICSI: Used when sperm need extra help (low count or poor movement), it’s a direct assist from the lab team.
About 70% of mature eggs fertilize successfully, turning into embryos over the next day or two. The embryologist watches them closely, checking for healthy growth.
A New Angle
Here’s something you might not read everywhere: labs are starting to use time-lapse imaging to monitor embryos without disturbing them. A 2024 trial from the University of Toronto showed this tech boosts embryo selection accuracy by 15%, giving doctors a better shot at picking winners.
Interactive Quiz: Which Method Suits You?
Answer these quick questions:
- Does your partner have a low sperm count? (Yes/No)
- Are you using donor sperm? (Yes/No)
- Have past IVF attempts failed to fertilize? (Yes/No)
If you said “Yes” to any, ICSI might be in your future. Chat with your doc to confirm!
Step 5: Growing the Embryos
Once fertilized, the embryos need a few days to grow—usually 3 to 5 days. They’re kept in a special incubator that mimics the womb, with just the right warmth and nutrients. By day 3, they’re at the “cleavage stage” (6-8 cells). By day 5, the healthiest ones reach the “blastocyst stage” (about 100 cells), which is prime time for transfer.
What’s Happening
The embryologist grades the embryos based on how they look—shape, size, and cell division. Not all make it to blastocyst, and that’s okay—it’s nature’s way of sorting the strong from the weak.
Fresh Insight
A hot topic in 2025? Preimplantation genetic testing (PGT). It’s not standard, but some folks use it to screen embryos for genetic issues before transfer. A recent Reproductive Sciences article found PGT bumps live birth rates by 10% for women over 37, though it’s pricey—around $3,000 extra.
Your Role
- ✔️ Ask your clinic how many embryos they expect to transfer.
- ❌ Don’t stress if some don’t grow—it’s part of the process.
- ✔️ Freeze extras for later cycles if you can.
Step 6: Embryo Transfer—The Homecoming
Time to bring the embryos home! This step is quick and painless—no anesthesia needed. The doctor slides a thin tube (catheter) through your cervix and places one or two embryos into your uterus. You’ll lie still for a bit after, then head home to wait.
The Details
- Timing: Usually day 3 or 5, depending on embryo growth.
- Number: One is common to avoid twins, but your doc might suggest two based on age or history.
- Feel: Like a Pap smear—mild pressure, that’s it.
Cool Twist
Ever heard of “mock transfers”? Some clinics do a practice run before the real deal to map your uterus. A 2024 study from Mayo Clinic showed this cuts transfer mishaps by 12%, especially for tricky cases.
Aftercare
- ✔️ Take it easy for a day—think Netflix, not marathons.
- ❌ No heavy lifting or hot tubs for 48 hours.
- ✔️ Sip water—your uterus loves hydration.
Step 7: The Two-Week Wait
Now, the hardest part: waiting. About 10-14 days after transfer, you’ll take a pregnancy test at the clinic. This “two-week wait” (TWW) is a rollercoaster—hope, nerves, and everything in between.
What’s Going On
The embryo needs to implant in your uterine lining. If it sticks, it starts releasing hCG—the pregnancy hormone your test will detect. About 40-55% of transfers lead to a positive test for women under 35, per CDC stats.
Coping Tips
- ✔️ Distract yourself with light hobbies—puzzles, anyone?
- ❌ Avoid home tests early—they can mislead you.
- ✔️ Lean on a friend who gets it—support is gold.
Poll Time: How Do You Wait?
What’s your TWW survival trick?
- A) Binge-watch a new show
- B) Journal every feeling
- C) Ignore it and hope for the best
Drop your pick in your mind—and hey, it might spark an idea!
Success Rates: What’s Realistic?
IVF isn’t a sure thing, but it’s got a solid track record. Success depends on age, egg quality, and a dash of luck. Here’s a peek at 2022 CDC numbers for first-cycle live births:
- Under 35: ~55%
- 35-37: ~40%
- 38-40: ~26%
- Over 40: ~8%
Fresh Take
A lesser-known stat: repeat cycles boost your odds. A 2023 Human Reproduction study found that after three cycles, cumulative success hits 65% for women under 38. So, one try isn’t the whole story.
Boost Your Chances
- ✔️ Eat a balanced diet—think Mediterranean vibes (fish, nuts, veggies).
- ❌ Skip the stress—yoga beats panic every time.
- ✔️ Sleep well—7-8 hours keeps your body happy.
Risks and Realities
IVF is safe, but it’s not risk-free. OHSS can happen if your ovaries overreact to meds, causing swelling and discomfort (rare, under 5%). Multiple births (twins+) are another risk if more than one embryo implants—about 15% of IVF pregnancies. And yes, miscarriage rates mirror natural ones—15-20%.
Under-the-Radar Concern
Something not always covered: emotional toll. A 2024 survey by Resolve found 60% of IVF patients felt “overwhelmed” at some point. Clinics are now offering free counseling—ask if yours does.
Stay Grounded
- ✔️ Talk to your partner or a pro if it gets heavy.
- ❌ Don’t bottle it up—feelings need air too.
- ✔️ Celebrate small wins, like finishing the shots.
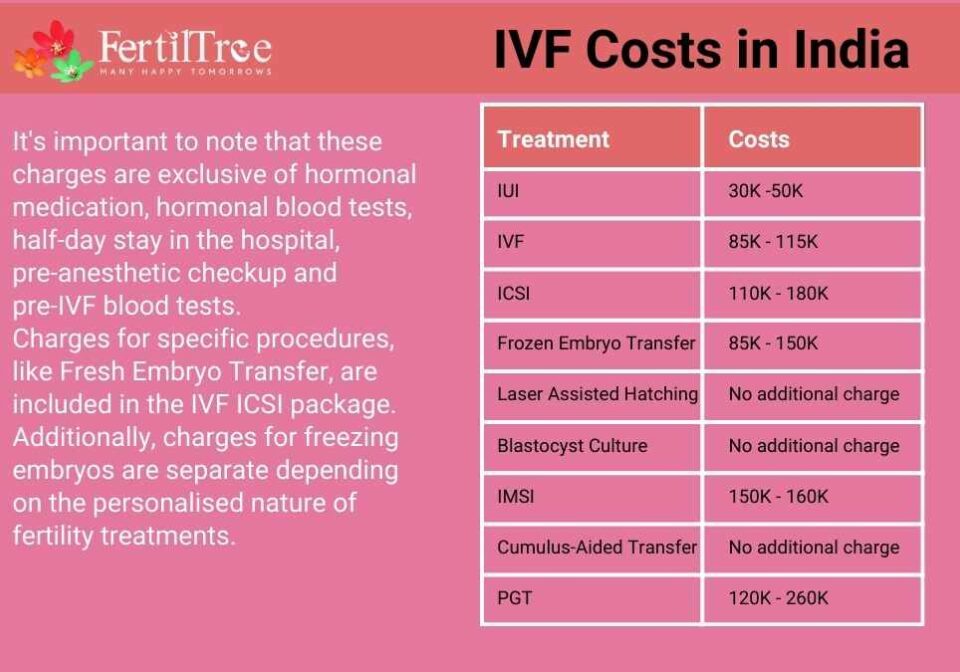
Costs: Breaking It Down
IVF isn’t cheap—$15,000-$20,000 per cycle in the U.S., including meds and lab fees. Insurance varies by state; only 19 mandate some coverage. Freezing embryos for later? Add $1,000-$2,000.
Hidden Gem
Mini-IVF, a lower-dose option, costs $5,000-$7,000 and works well for some. A 2024 Journal of Assisted Reproduction report showed it’s 80% as effective for women with good ovarian reserve—worth a look if budgets are tight.
Money-Saving Hacks
- ✔️ Check for clinic discounts or payment plans.
- ❌ Don’t skip consults—free ones can clarify costs.
- ✔️ Look into grants—groups like BabyQuest offer aid.
The Future of IVF: What’s Next?
IVF keeps evolving. In 2025, we’re seeing buzz around artificial intelligence picking the best embryos (upping success by 10%, per a Stanford study) and “in vitro gametogenesis”—making eggs or sperm from skin cells. It’s still experimental, but it could change the game for folks with no viable gametes.
Untapped Topic: Mental Prep
One thing missing from most guides? Pre-IVF mindset work. A 2024 pilot program at Yale Fertility Center had patients do mindfulness sessions before starting. Result? 25% less anxiety during the TWW. Try a 5-minute breathing exercise daily—inhale 4 seconds, hold 4, exhale 4.
Real Stories: Voices of IVF
Meet Sarah, 34, who did IVF after three years of trying naturally. “The shots were tough, but seeing those embryos on the screen? Unreal. My son’s two now—I’d do it all again.” Then there’s Mike, 41, a single dad via surrogacy. “IVF felt like a sci-fi movie, but holding my daughter made every penny worth it.”
Your Turn: Dream Big
Picture this: What would your IVF win look like? A nursery painted blue? Twins giggling in a stroller? Hold that image—it’s fuel for the journey.
Wrapping It Up
IVF is a marathon, not a sprint—a blend of science, grit, and a little bit of wonder. From priming your ovaries to that nail-biting wait, every step builds toward possibility. It’s not perfect, and it’s not easy, but it’s a path millions have walked to meet their kids. If you’re on this road, know you’re not alone—there’s a whole community cheering you on. And if you’re just curious, now you’ve got the full scoop—plus a few extras to impress your friends. What’s your next step? Maybe it’s a chat with a doctor, a deep breath, or just soaking in the hope. Whatever it is, you’ve got this.