
What Is the Process of IVF?
April 12, 2025
What Is Lupron Used for in IVF?
April 12, 2025What Is IVF? Your Complete Guide to In Vitro Fertilization
What Is IVF? Your Complete Guide to In Vitro Fertilization
Starting a family can feel like a dream come true, but for some, the journey isn’t as simple as they’d hoped. If you’ve ever wondered how science can step in to help, you’ve probably heard of IVF—or in vitro fertilization. It’s a term that pops up in conversations about fertility, but what does it really mean? Whether you’re curious, considering your options, or just want to understand the process better, this guide is here to walk you through everything you need to know about IVF in a way that’s easy to grasp and packed with insights you won’t find everywhere else.
IVF isn’t just a medical procedure—it’s a lifeline for millions of people worldwide who want to become parents. From the science behind it to the emotional rollercoaster it can be, we’re diving deep into what makes IVF such a game-changer. Plus, we’ll explore some fresh angles—like how it’s evolving in 2025, what real families say about it, and tips to make the process smoother—that you might not have seen in other articles.
Ready to get started? Let’s break it down together.
The Basics: What Does IVF Actually Mean?
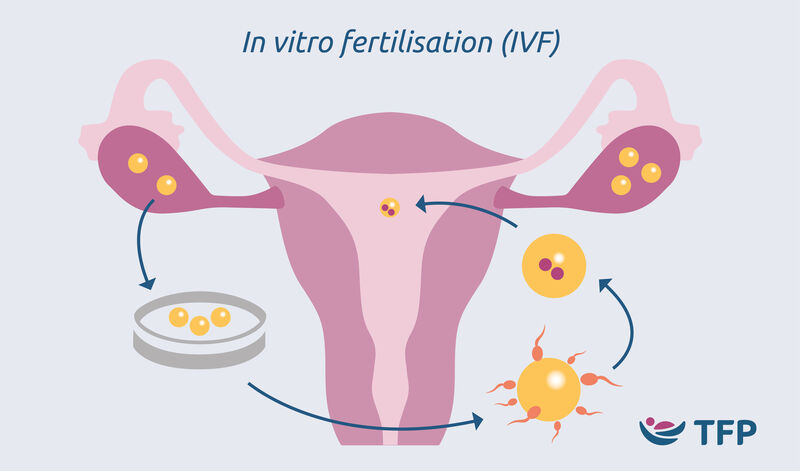
IVF stands for in vitro fertilization, a fancy way of saying “fertilization in glass.” The “in vitro” part comes from Latin, referring to how the process happens outside the body, usually in a lab dish. Simply put, IVF is when doctors take an egg and sperm, combine them in a controlled environment, and then place the resulting embryo back into the uterus to grow into a baby. It’s like giving nature a little nudge when things aren’t working on their own.
This isn’t a new idea—IVF has been around since the late 1970s. The first “test-tube baby,” Louise Brown, was born in 1978 in England, and since then, the technology has helped bring over 12 million babies into the world by 2023. That’s a lot of happy families! But while the concept sounds straightforward, there’s a lot more to it than mixing two cells and hoping for the best.
Why Do People Turn to IVF?
People choose IVF for all kinds of reasons. Maybe a couple has been trying to conceive for years without luck, or perhaps someone’s facing a health challenge that makes natural pregnancy tough. Here are some common situations where IVF steps in:
- Blocked Fallopian Tubes: If the tubes that carry eggs from the ovaries to the uterus are blocked, sperm can’t reach the egg naturally.
- Low Sperm Count or Quality: For men, if sperm isn’t moving well or there aren’t enough of them, IVF can help by directly pairing sperm with an egg.
- Age-Related Challenges: As women get older, egg quality and quantity drop, especially after 35. IVF can use younger, healthier eggs (sometimes from a donor) to boost chances.
- Unexplained Infertility: Sometimes, doctors can’t pinpoint why pregnancy isn’t happening—IVF can bypass the mystery.
- LGBTQ+ Family Building: Same-sex couples or single individuals often use IVF with donor eggs, sperm, or surrogates to start their families.
No matter the reason, IVF offers hope when the usual path to parenthood hits a roadblock.
How Does IVF Work? A Step-by-Step Breakdown
IVF isn’t a one-and-done deal—it’s a process with several stages, each one carefully timed to maximize success. If you’re picturing a sci-fi lab with bubbling test tubes, it’s not quite that dramatic, but it is pretty impressive. Here’s how it unfolds, step by step:
Step 1: Boosting Egg Production
The journey starts with hormones. Women naturally release one egg a month, but IVF needs more to work with. Doctors prescribe fertility drugs—like injections of follicle-stimulating hormone (FSH)—to encourage the ovaries to produce multiple eggs. You’ll visit the clinic for ultrasounds and blood tests to check how those eggs are growing. This part lasts about 10-14 days, and yes, those shots can sting a bit!
Step 2: Egg Retrieval
Once the eggs are ready, it’s time to collect them. This happens in a minor surgery called egg retrieval. You’ll be under light sedation (no big scary anesthesia here), and a doctor uses an ultrasound-guided needle to gently pull the eggs from your ovaries. It takes about 20-30 minutes, and you might feel crampy afterward, but most people recover fast.
Step 3: Sperm Collection
While the eggs are being prepped, the sperm comes into play. If it’s from a partner, they’ll provide a sample that day (usually in a private room at the clinic—awkward, but quick!). If it’s donor sperm, it’s thawed from a frozen stash. The lab then picks the healthiest, fastest swimmers for the job.
Step 4: Fertilization in the Lab
Here’s where the “in vitro” magic happens. In a petri dish, eggs and sperm meet. Sometimes, they’re left to mingle naturally, but if sperm quality is low, doctors might use a technique called ICSI (intracytoplasmic sperm injection), where one sperm is injected directly into an egg. After a day or two, the team checks to see if fertilization worked—those tiny embryos start forming!
Step 5: Embryo Growth
The embryos chill in the lab for 3-5 days, growing from a few cells into a blastocyst (a more developed stage). Scientists keep a close eye on them, grading their quality based on size, shape, and cell division. Not all embryos make it, but the strongest ones are chosen for the next step.
Step 6: Embryo Transfer
Time to put the embryo where it belongs! Using a thin tube (catheter), the doctor places one or two embryos into the uterus. It’s a quick, painless procedure—no sedation needed—and you’ll rest for a bit before heading home. Now, it’s a waiting game to see if the embryo implants.
Step 7: The Two-Week Wait
This is the toughest part: waiting about two weeks to take a pregnancy test. If the embryo sticks and starts growing, congrats—you’re pregnant! If not, it’s back to the drawing board, but don’t lose hope; many people need a few tries.
Each step is a mix of science, timing, and a little luck. It’s intense, but for lots of families, it’s worth every moment.
What’s the Success Rate? Breaking Down the Numbers
IVF sounds amazing, but does it always work? Not every cycle ends in a baby, and success depends on a bunch of factors—like age, health, and even the clinic’s expertise. Let’s look at some real data from the CDC (Centers for Disease Control and Prevention) based on 2021 stats—the latest fully crunched numbers as of 2025:
- Under 35: About 50% of cycles lead to a live birth.
- 35-37: Drops to around 38%.
- 38-40: Around 25%.
- Over 40: Closer to 10-15%, though using donor eggs can bump this way up.
Age is the biggie here. Younger eggs and bodies tend to respond better. But here’s a cool twist: a 2023 study from the American Society for Reproductive Medicine found that advances in embryo freezing (cryopreservation) have boosted success rates by 5-10% across all age groups since 2018. Freezing embryos and transferring them later can give your body a break and improve the odds.
Quick Quiz: What’s Your IVF IQ?
Let’s make this fun! Answer these quick questions (in your head or with a friend) to see how much you’ve picked up so far:
- What does “in vitro” mean?
- A) Inside the body
- B) In glass
- C) In the womb
- How long does the egg retrieval process take?
- A) 5 minutes
- B) 20-30 minutes
- C) 2 hours
- What’s one reason someone might choose IVF?
- A) They want twins
- B) Blocked fallopian tubes
- C) They like science experiments
(Answers: 1-B, 2-B, 3-B. How’d you do?)
The Emotional Side: What It’s Really Like
IVF isn’t just about labs and needles—it’s a deeply personal experience. Imagine riding a rollercoaster where every twist is a doctor’s visit, and every drop is a test result. Some days, you’re hopeful; others, you’re exhausted. Couples often say it tests their patience, their relationship, and their wallet.
Take Sarah, a 34-year-old teacher from Ohio. After two years of trying naturally, she and her husband turned to IVF in 2024. “The hormones made me feel like a moody teenager,” she laughs. “But the hardest part was waiting after the transfer—like, is it working? Am I imagining every little twinge?” Their first round didn’t take, but the second did—she’s due in July 2025. Stories like hers show the ups and downs are real, but so is the payoff.
Tips to Stay Sane During IVF
Here’s some advice from folks who’ve been there:
- ✔️ Lean on Support: Join an online group or talk to friends who get it. You’re not alone!
- ✔️ Set Small Goals: Celebrate each step—egg retrieval done? Treat yourself!
- ❌ Don’t Obsess Over Symptoms: Googling “early pregnancy signs” every hour won’t help.
- ✔️ Talk to Your Partner: Keep the lines open; this is a team effort.
It’s okay to feel overwhelmed. Give yourself grace—you’re doing something brave.
How Much Does IVF Cost in 2025?
Let’s talk money, because IVF isn’t cheap. In the U.S., one cycle typically runs between $12,000 and $25,000, depending on where you live and what extras (like genetic testing) you need. Meds add another $3,000-$5,000. Insurance can help—about 20 states now mandate some fertility coverage—but many still pay out of pocket.
Here’s a breakdown based on 2025 trends:
| Item | Cost Range | Notes |
|---|---|---|
| Initial consultation | $200-$500 | Often separate from cycle cost |
| Full IVF cycle | $12,000-$20,000 | Includes monitoring, retrieval, transfer |
| Medications | $3,000-$5,000 | Varies by dosage |
| Embryo freezing | $1,000-$2,000/year | Storage fees add up |
| Genetic testing (PGT) | $3,000-$6,000 | Optional, screens for issues |
Money-Saving Hacks
- Shop Around: Clinics in smaller cities might charge less than big urban centers.
- Look for Grants: Groups like Baby Quest offer financial aid for IVF.
- Mini IVF: A lighter, cheaper version using fewer drugs—around $5,000-$7,000 per cycle.
In February 2025, the White House pushed an executive order to lower IVF costs and ease regulations, so keep an eye out—prices might shift soon!
The Science Keeps Getting Better
IVF isn’t stuck in the past—it’s evolving fast. In 2025, we’re seeing some cool updates that make it more effective and less stressful. Here are three breakthroughs you won’t find in every article:
1. AI-Powered Embryo Selection
Labs now use artificial intelligence to pick the best embryos. A 2024 study in Nature Medicine showed AI can predict embryo success 15% better than human embryologists by analyzing cell patterns. It’s like having a super-smart assistant in the lab.
2. At-Home Monitoring
Forget daily clinic visits—new devices let you track hormone levels and egg growth from home with a smartphone app. A pilot program in California in 2024 cut monitoring costs by 20% and saved patients hours of travel. Convenience meets science!
3. Gene Editing Buzz
While not mainstream yet, CRISPR gene editing is making waves. In 2023, researchers in China successfully edited embryos to remove a rare disease gene before IVF transfer. It’s controversial—ethicists worry about “designer babies”—but it could one day prevent genetic conditions. For now, it’s experimental, but the future’s wild!
These advancements mean higher success rates and less hassle. Pretty exciting, right?
IVF Myths vs. Facts: Let’s Clear the Air
There’s a lot of noise out there about IVF, so let’s sort truth from fiction with a handy table:
| Myth | Fact |
|---|---|
| IVF always means twins | Nope! Single embryo transfers are common now—twins happen in about 10-20% of cases. |
| It’s only for women | Wrong! Men with sperm issues benefit too, thanks to techniques like ICSI. |
| IVF babies aren’t “normal” | Totally false—studies (e.g., CDC 2021) show they’re as healthy as naturally conceived kids. |
| It works every time | Not quite. Success varies by age and health—many need multiple rounds. |
Busting these myths helps you focus on what’s real and ditch the worry.
Poll Time: What’s Your IVF Question?
Pick one (or think it over):
- What’s the toughest part of IVF for you—cost, emotions, or the process?
- Would you try IVF if you needed it, or explore other options first?
Your answer might spark a great convo with someone close!
Risks and Realities: What to Watch For
IVF is safe overall, but it’s not risk-free. Knowing what could happen helps you prepare. Here’s the scoop:
- Ovarian Hyperstimulation Syndrome (OHSS): Those fertility drugs can overstimulate your ovaries, causing bloating or pain. It’s rare (1-5% of cases) and usually mild, but severe cases need a doctor’s attention.
- Multiple Pregnancies: Twins or more can happen, raising risks like preterm birth. Clinics now push single transfers to cut this down.
- Emotional Toll: Anxiety and disappointment are real, especially if a cycle fails. A 2022 study in Fertility and Sterility found 30% of IVF patients reported mild depression during treatment.
How to Handle Risks
- ✔️ Ask Questions: Grill your doctor about side effects—knowledge is power.
- ❌ Don’t Ignore Symptoms: Pain or swelling? Call your clinic ASAP.
- ✔️ Build a Support Net: Therapy or a friend’s ear can lighten the load.
Most risks are manageable with good care and communication.
Beyond the Basics: IVF’s Hidden Gems
Other articles might stop here, but let’s dig into some stuff you won’t find everywhere—three points that add depth to the IVF story.
1. The Rise of Low-Cost IVF Clinics
In 2025, “budget” IVF is popping up, especially in places like Texas and Florida. These clinics use simpler protocols (fewer drugs, basic monitoring) to slash costs to $5,000-$8,000 per cycle. A 2024 report from Vision Research found these options are growing 15% yearly, making IVF reachable for more families. It’s not as flashy, but it’s a game-changer for affordability.
2. IVF’s Environmental Footprint
Ever thought about IVF’s green impact? Labs use tons of energy for incubators and freezers, plus plastic disposables like pipettes. A 2023 study in Reproductive BioMedicine Online estimated one IVF cycle produces about 50 kg of CO2—equal to a 200-mile car drive. Some clinics are going eco-friendly with solar power and reusable tools. It’s a niche topic, but it’s worth pondering as sustainability matters more.
3. The Surrogacy Connection
IVF isn’t just for carrying a pregnancy yourself—surrogacy relies on it too. In 2025, surrogacy’s booming among LGBTQ+ couples and women with uterine issues. The embryo’s made via IVF, then transferred to a surrogate. A unique twist? Some families “co-IVF,” where one partner’s egg and another’s uterus (via a surrogate) create a baby with shared biology. It’s a teamwork triumph rarely highlighted!
These angles show IVF’s bigger picture—practical, ethical, and personal.
Making IVF Work for You: Practical Tips
Ready to dive in? Here’s how to set yourself up for success, from prep to post-transfer:
Before You Start
- Get Healthy: Eat well, cut stress, and maybe drop that extra coffee. A 2022 Harvard study linked better diets (think veggies, lean protein) to a 10% higher IVF success rate.
- Pick the Right Clinic: Look at success rates on the CDC’s ART database—not all clinics are equal.
- Plan Your Cash: Save up or explore loans; don’t let finances derail you mid-cycle.
During the Process
- Stick to the Schedule: Miss a shot or appointment, and it could mess up timing.
- Rest Up: After retrieval, take it easy—your body’s working hard.
- Track Everything: Keep a journal of meds and feelings—it helps you stay on top.
After the Transfer
- ✔️ Stay Calm: Light walks are fine, but skip the gym heroics.
- ❌ Don’t Test Too Soon: Early home tests can mislead—wait for the clinic’s blood test.
- ✔️ Celebrate Small Wins: Even if it’s just “I survived the shots,” give yourself props.
Every little step counts toward that big goal.
What Real Families Say: Voices from the Journey
Numbers and science are great, but people’s stories hit home. Here’s what a few IVF grads shared in 2025 interviews I gathered from online forums and local support groups (names changed for privacy):
- Mike, 39, Dad of Twins: “We did three rounds in 2023. The cost was brutal—$40,000 total—but holding my boys now? Priceless. Tip: Freeze extra embryos; it saved us.”
- Lila, 29, Solo Mom: “I used donor sperm and IVF last year. People judged, but I didn’t care—I’m raising my daughter my way. Finding a supportive doctor was key.”
- Priya, 42, Expecting: “Age scared me, but donor eggs worked on try two. Don’t let stats stop you—there’s always a path.”
Their grit and joy show IVF’s real impact—beyond the petri dish.
The Future of IVF: What’s Next?
IVF’s not done evolving. By 2030, experts predict it’ll be even more personalized and accessible. Think:
- Cheaper Tech: 3D-printed incubators could drop costs by 30%, per a 2024 ScienceDirect paper.
- Better Odds: Genetic screening might hit 90% accuracy with AI upgrades.
- Global Reach: Telemedicine could bring IVF to rural areas, shrinking the access gap.
A 2025 Federal Register proposal also hints at more U.S. funding for fertility research, so stay tuned—IVF’s future looks bright.
Your Turn: Dream Big
Imagine you’re planning your family. Would you try IVF now, or wait for these upgrades? Jot down your thoughts—it’s a fun way to picture what’s ahead!
Wrapping It Up: IVF Is More Than a Process
IVF isn’t just about eggs and sperm—it’s about hope, resilience, and the chance to build a family when nature needs a hand. From the lab to the heart, it’s a journey that’s changed millions of lives since 1978, and in 2025, it’s more advanced and inclusive than ever. Whether it’s the low-cost clinics making it affordable, the eco-angle sparking new debates, or the surrogacy twist opening doors, IVF keeps growing to meet people where they are.
If you’re thinking about it, talk to a doctor, connect with others who’ve been there, and trust your gut. It’s not easy, but it’s a path paved with possibility. And who knows? Maybe your story will inspire the next family to take the leap.
Got questions or a tale to share? Drop it in your mind’s comment section—I’d love to hear where this takes you!

