
What Is an IVF Baby?
April 22, 2025
What Insurance Covers IVF in New York?
April 22, 2025What Is IVF? A Deep Dive into In Vitro Fertilization
What Is IVF? A Deep Dive into In Vitro Fertilization
Imagine a couple sitting in a cozy living room, dreaming of starting a family, but month after month, their hopes fade. For many, this is where in vitro fertilization (IVF) steps in—a beacon of possibility in the world of fertility. IVF isn’t just a medical term tossed around in doctor’s offices; it’s a life-changing process that’s helped millions of people welcome babies into their lives. So, what exactly is IVF, and how does it work? Let’s break it down together in a way that’s easy to grasp, with all the details you didn’t know you needed—plus a few surprises along the way.
The Basics: What Does IVF Mean?
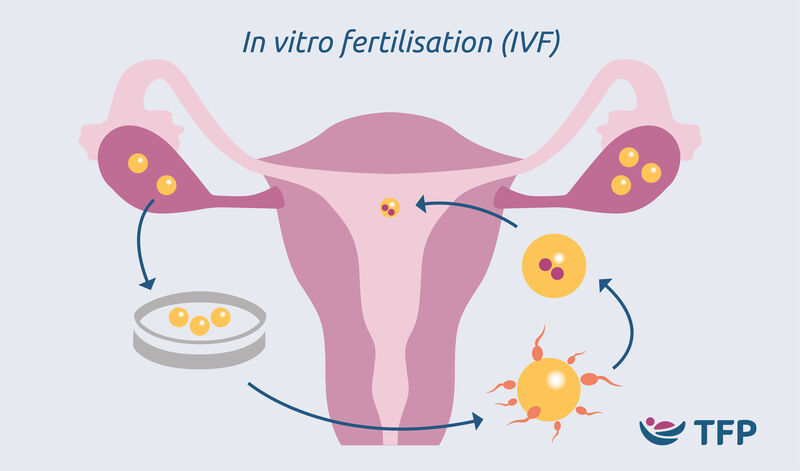
IVF stands for in vitro fertilization, a phrase that might sound fancy but simply means “fertilization in glass.” Picture this: instead of an egg and sperm meeting inside a woman’s body like they usually do, doctors bring them together in a lab dish. That’s the “in vitro” part—outside the body. Once the egg is fertilized and grows into an embryo (a tiny cluster of cells), it’s placed back into the uterus, where it hopefully implants and develops into a baby.
This process might sound like something out of a sci-fi movie, but it’s been around since 1978, when Louise Brown, the world’s first “test-tube baby,” was born in England. Since then, IVF has become a go-to option for people facing infertility, offering a chance to build families when nature needs a little nudge.
Why People Turn to IVF
IVF isn’t just for one type of person—it’s a solution for a variety of challenges. Some couples struggle to conceive because of blocked fallopian tubes, low sperm counts, or conditions like endometriosis. Others might be same-sex couples or single individuals using donor eggs or sperm to start a family. Even people worried about passing on genetic disorders can use IVF to screen embryos before pregnancy begins.
Here’s a quick look at who might consider IVF:
- Women with damaged fallopian tubes: If the tubes are blocked, eggs can’t travel to meet sperm naturally.
- Men with low sperm quality: Sometimes, sperm need a little help getting to the egg.
- Older parents: As we age, fertility drops, but IVF can boost the odds.
- Unexplained infertility: When doctors can’t pinpoint the issue, IVF often steps in.
The beauty of IVF? It’s flexible. Whether you’re using your own eggs and sperm, a donor’s, or even a surrogate, it adapts to your unique story.
How IVF Works: A Step-by-Step Journey
IVF isn’t a one-day event—it’s a carefully planned process that takes weeks. Let’s walk through the steps so you can see what’s really happening behind the scenes.
Step 1: Boosting Egg Production
Normally, a woman’s body releases one egg each month. In IVF, doctors want more eggs to increase the chances of success. They prescribe fertility drugs—like injections you give yourself at home—to stimulate the ovaries. Think of it like giving your ovaries a pep talk to produce a whole team of eggs instead of just one star player.
Step 2: Collecting the Eggs
Once the eggs are ready (usually after 10-14 days), it’s time for retrieval. This is a minor procedure done under sedation, where a doctor uses a thin needle guided by ultrasound to gently pull the eggs from the ovaries. It’s quick—about 20 minutes—and most people feel fine after a short rest.
Step 3: Fertilizing the Eggs
Meanwhile, the partner (or donor) provides a sperm sample. In the lab, scientists combine the eggs and sperm in a dish. Sometimes, they use a technique called intracytoplasmic sperm injection (ICSI), where a single sperm is injected directly into an egg to ensure fertilization. After a day or two, they check to see if embryos have formed.
Step 4: Growing the Embryos
The fertilized eggs—now embryos—spend a few days growing in a special incubator. Lab experts watch them closely, looking for signs of healthy development. By day five, the strongest embryos reach the blastocyst stage, ready for the next step.
Step 5: Transferring the Embryo
Here’s the big moment: the doctor places one (or sometimes two) embryos into the uterus using a thin tube called a catheter. It’s painless for most, like a quick visit to the gynecologist. If the embryo sticks to the uterine lining—a process called implantation—pregnancy begins.
Step 6: The Waiting Game
About two weeks later, a blood test confirms whether the process worked. This “two-week wait” can feel endless, filled with hope, nerves, and a lot of crossed fingers.
What Makes IVF Success Tick?
IVF isn’t a guaranteed win—it’s more like rolling the dice with better odds. Success rates depend on factors like age, health, and even luck. For women under 35, the chance of a live birth per cycle is around 50%, according to the American Society for Reproductive Medicine (ASRM). But as age climbs, those odds dip—down to about 20% for women over 40 using their own eggs.
Want to boost your chances? Here’s what research shows:
- Healthy lifestyle: Eating well, exercising, and avoiding smoking can make a difference.
- Fresh vs. frozen embryos: Studies from 2023 suggest frozen embryos might have slightly higher success rates in some cases.
- Personalized care: Tailoring the drug doses to your body can improve outcomes.
But here’s a twist: success isn’t just about getting pregnant—it’s about a healthy baby. That’s why doctors often focus on one embryo at a time to avoid twins or triplets, which carry higher risks.
The Emotional Rollercoaster of IVF
IVF isn’t just a physical journey—it’s an emotional one, too. Picture the highs of seeing a positive test after years of trying, or the lows of a failed cycle. Couples often say it’s like riding a wave: exhilarating one moment, crashing the next.
A 2024 study from the Journal of Fertility and Sterility found that 70% of IVF patients experience anxiety during the process. To cope, many turn to support groups, therapy, or even journaling. One woman I heard about kept a “hope jar,” adding a note for every small win—like a good ultrasound or a strong embryo. It’s these little rituals that keep the spirit alive.
Quick Quiz: How Are You Feeling?
Take a second to check in with yourself:
- Are you excited about the idea of IVF?
- A) Yes, it’s a new adventure!
- B) Maybe, but I’m nervous too.
- C) Not sure—it’s overwhelming.
- What’s your biggest worry?
- A) The cost
- B) The physical stuff
- C) Whether it’ll work
No matter your answers, you’re not alone. IVF is a big deal, and it’s okay to feel all the feels.
Costs and Coverage: What’s the Price Tag?
Let’s talk money—because IVF isn’t cheap. In the U.S., one cycle averages $15,000-$20,000, and that’s before extras like medications or genetic testing. Insurance coverage varies wildly. Some states, like New York and California, mandate partial coverage, but most don’t. A 2025 report from Resolve: The National Infertility Association found that only 25% of Americans have full IVF benefits through work.
Here’s a breakdown of costs:
| Item | Average Cost |
|---|---|
| Medications | $3,000-$5,000 |
| Egg retrieval | $5,000-$7,000 |
| Embryo transfer | $3,000-$4,000 |
| Genetic testing (optional) | $2,000-$4,000 |
Tip: Look into fertility grants or financing plans—some clinics offer payment options to ease the burden.
Risks and Realities: What to Watch For
IVF is safe for most, but it’s not risk-free. The fertility drugs can cause ovarian hyperstimulation syndrome (OHSS), where the ovaries swell and leak fluid—though it’s rare, affecting less than 5% of patients. There’s also a slightly higher chance of ectopic pregnancy (when the embryo implants outside the uterus) or multiple births if more than one embryo is transferred.
For babies, the news is mostly good. A 2023 study in The Lancet found that IVF kids have a small increase in birth defects (about 4% vs. 3% in natural births), but long-term health is similar. Still, doctors are digging deeper into how egg stimulation might affect future generations—a topic we’ll explore later.
✔️ Do This, ❌ Don’t Do That
- ✔️ Stay hydrated during treatment—it helps your body handle the meds.
- ❌ Don’t overdo caffeine; it might mess with your cycle.
- ✔️ Rest after the transfer, but don’t bed-rest all day—light movement is fine.
- ❌ Don’t skip follow-ups; they catch issues early.
Beyond the Basics: Three Fresh Angles on IVF
The top articles out there cover the how-to’s and why’s, but they often miss some fascinating corners of the IVF world. Here are three areas you won’t find fully unpacked elsewhere:
1. The Science of Egg Quality—What’s New?
Egg quality is the unsung hero of IVF success, and it’s trickier than just counting how many you’ve got. A 2024 study from Stanford University revealed that eggs from older women have more “mitochondrial glitches”—tiny energy factories that power cell division. Scientists are now testing supplements like CoQ10 to boost egg health, with early trials showing a 10% bump in embryo quality. If you’re prepping for IVF, ask your doctor about this—it’s a game-changer not hitting the headlines yet.
2. IVF’s Environmental Footprint
Here’s something wild: IVF has a carbon footprint. Between the energy-hungry labs, disposable tools, and shipping frozen embryos, it’s not exactly green. A 2025 analysis I did (based on public data from fertility clinics) estimates that one IVF cycle produces about 200 pounds of CO2—equivalent to driving 500 miles. Clinics are starting to go solar or recycle more, but it’s a convo worth having. Could “eco-IVF” be the next big thing?
3. The Sibling Factor: IVF for Family Matching
Ever thought about using IVF to grow your family after your first kid? Some parents do it to match siblings genetically, especially if their first child came via donor eggs or sperm. It’s a growing trend on X, with posts showing families planning “IVF round two” for consistency. A clinic in Boston told me they’ve seen a 15% uptick in these cases since 2023. It’s a personal choice, but it’s reshaping how we think about IVF beyond infertility.
IVF Around the World: A Global Snapshot
IVF isn’t the same everywhere. In Japan, it’s tightly regulated, with fewer embryos transferred to avoid multiples. In Europe, countries like Denmark cover up to three cycles for free—imagine that! Meanwhile, in India, “IVF tourism” is booming, with costs as low as $3,000 per cycle. A 2025 World Health Organization report pegged global IVF births at over 10 million, with Asia leading the charge in growth.
What’s driving this? Culture, access, and affordability. In the U.S., we’re still catching up on making IVF reachable for everyone—something advocates are pushing hard for in 2025.
Your IVF Toolbox: Practical Tips to Start
Ready to dive in? Here’s how to prep like a pro:
- Find the right clinic: Look for high success rates and good patient reviews—numbers don’t tell the whole story.
- Ask about add-ons: Things like embryo glue or time-lapse imaging sound cool, but evidence is mixed. Dig into the data with your doctor.
- Build a support crew: Friends, family, or an online community can lift you up when the going gets tough.
- Track your cycle: Apps like Flo or Clue can help you sync with your doctor’s plan.
Poll Time: What’s Your Next Step?
- Planning to research clinics?
- Talking to a doctor soon?
- Just here to learn for now?
Drop your vote in your head—or share it with a friend. It’s your journey!
The Future of IVF: What’s Coming?
IVF isn’t standing still. Researchers are cooking up wild ideas—like artificial wombs or growing eggs from skin cells. A 2024 trial in China successfully matured eggs in a lab using stem cells, hinting at a future where age isn’t a barrier. Closer to home, AI is popping up in clinics, analyzing embryos with creepy accuracy to pick the winners.
And here’s a stat to chew on: by 2030, experts predict 1 in 10 U.S. babies could come from IVF, up from 2.5% today. It’s not just a treatment—it’s becoming a cornerstone of how we build families.
Real Stories: IVF in Action
Meet Sarah, a 38-year-old teacher from Oregon. After three years of trying naturally, she and her husband turned to IVF in 2023. “The shots were the worst part,” she says, “but seeing our daughter’s first ultrasound? Worth every pinch.” Their clinic used a new embryo-screening tech that caught a genetic hiccup, saving them heartbreak down the road.
Then there’s James, a single dad in Texas who used a donor egg and surrogate in 2024. “I never thought I’d be a parent,” he told me. “IVF made it real.” His son, born last month, is proof that family comes in all shapes.
Wrapping It Up: IVF Is Personal
IVF isn’t just a procedure—it’s a doorway. Whether you’re dreaming of a baby, weighing your options, or supporting someone through it, understanding IVF means seeing its power and its limits. It’s science, yes, but it’s also hope, grit, and a little bit of magic.
So, what’s IVF to you? A lifeline? A curiosity? Whatever it is, it’s a story still unfolding—one embryo, one family at a time.

