
Is IVF in Mexico Safe? Your Guide to Making an Informed Choice
April 21, 2025
What Are the Long-Term Side Effects of IVF Injections?
April 21, 2025What Does IVF Stand for in Medical Terms?
What Does IVF Stand for in Medical Terms?
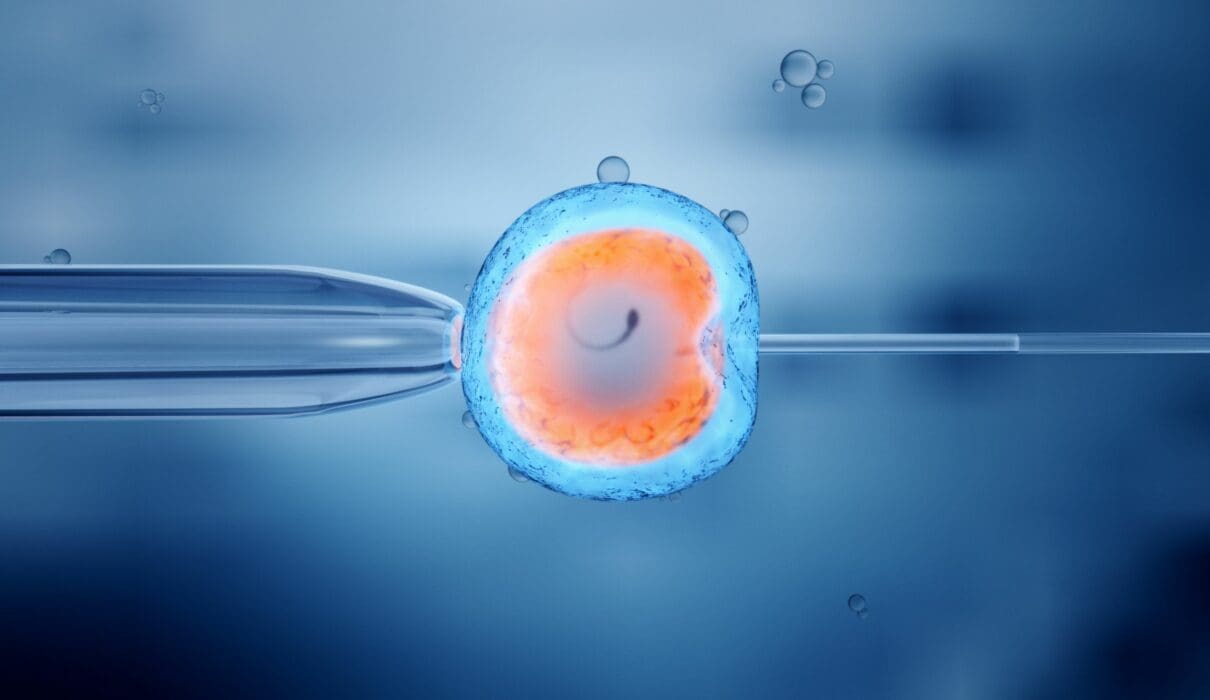
When someone mentions IVF, you might picture test tubes, doctors in lab coats, or maybe even a tiny miracle growing in a dish. But what does IVF actually stand for in medical terms, and why does it matter to so many people? IVF, or in vitro fertilization, is a process where a woman’s egg and a man’s sperm are combined outside the body—in a lab—before being placed into the uterus to grow into a baby. The phrase “in vitro” comes from Latin, meaning “in glass,” which nods to how this fertilization happens in a controlled environment, like a petri dish, rather than inside the body.
IVF isn’t just a science experiment; it’s a lifeline for millions who dream of starting a family but face roadblocks like infertility. Since the first IVF baby, Louise Brown, was born in 1978, this technology has evolved into a cornerstone of modern medicine, helping over 8 million babies come into the world. So, let’s dive into what IVF really means, how it works, and why it’s so much more than just a medical term—it’s a story of hope, science, and resilience.
The Basics: Breaking Down IVF Step by Step
IVF might sound complicated, but it’s really a series of steps that work together to make pregnancy possible when nature needs a nudge. Imagine it like baking a cake: you gather the ingredients (eggs and sperm), mix them in a special way (fertilization in a lab), and then put the batter in the oven (the uterus) to bake (grow into a baby). Here’s how it happens:
Step 1: Boosting Egg Production
A woman’s body usually releases one egg a month, but IVF cranks that up a notch. Doctors give you fertility drugs—think of them as super-charged hormones—to help your ovaries produce several eggs at once. You’ll get shots or pills for about 10-14 days, and the doctor will check your progress with ultrasounds and blood tests.
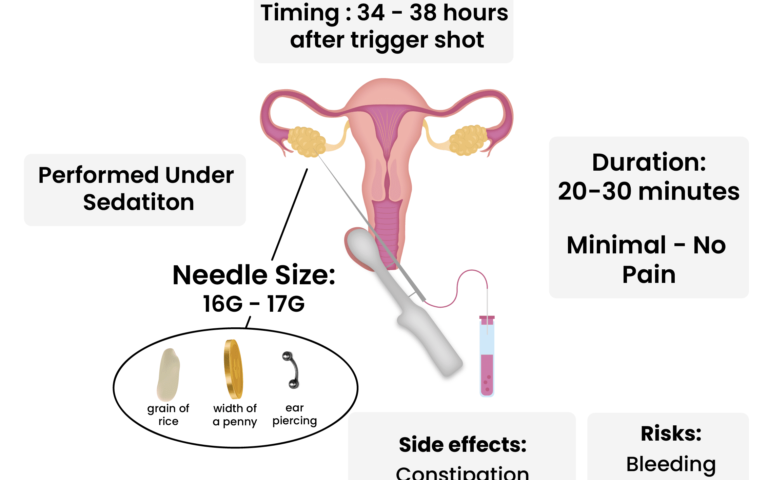
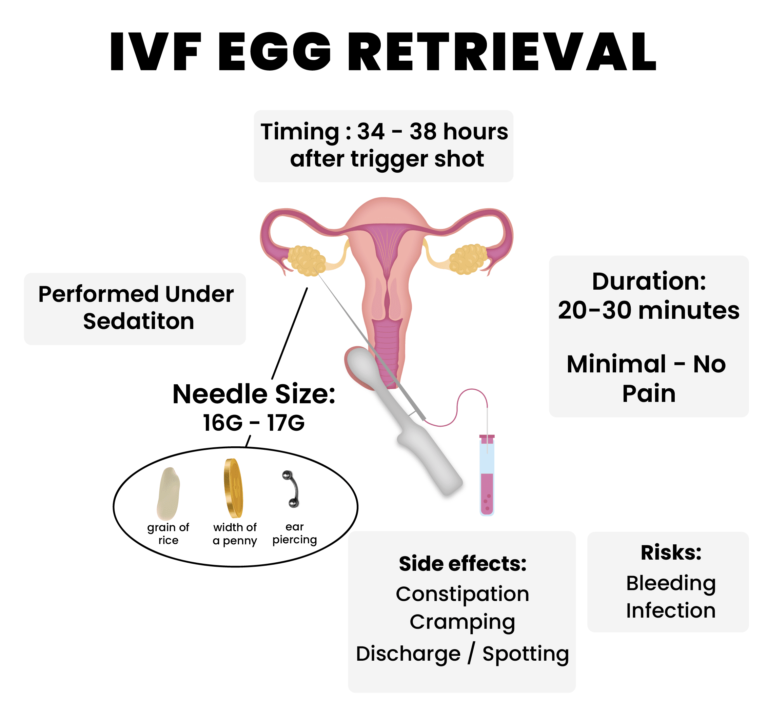
Step 2: Collecting the Eggs
Once those eggs are ready, it’s time to grab them. This is called egg retrieval, and it’s a quick procedure done under light sedation. A doctor uses a thin needle guided by ultrasound to gently pull the eggs from your ovaries. It takes about 20-30 minutes, and you’re awake but relaxed—no major surgery here!
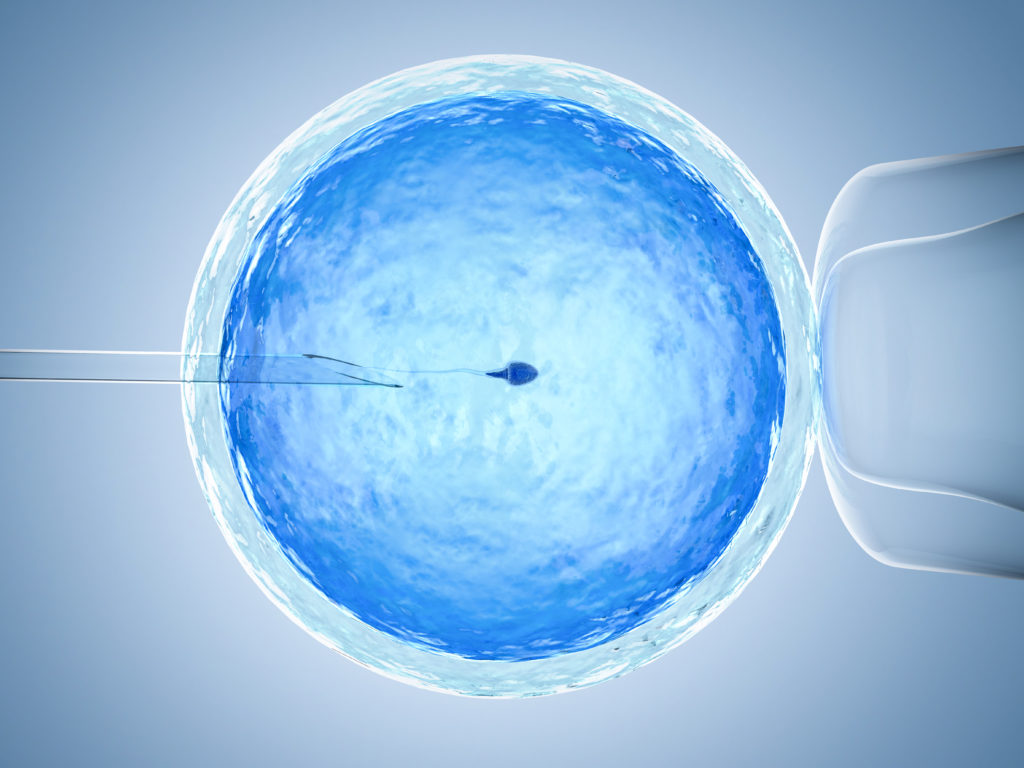
Step 3: Fertilizing the Eggs
Now comes the “in vitro” part. In a lab, the eggs meet the sperm—either from a partner or a donor. Sometimes, the sperm and eggs are just mixed together in a dish and left to do their thing. Other times, a scientist uses a tiny needle to inject a single sperm into an egg (this is called ICSI, or intracytoplasmic sperm injection). After a day or two, fertilized eggs become embryos.
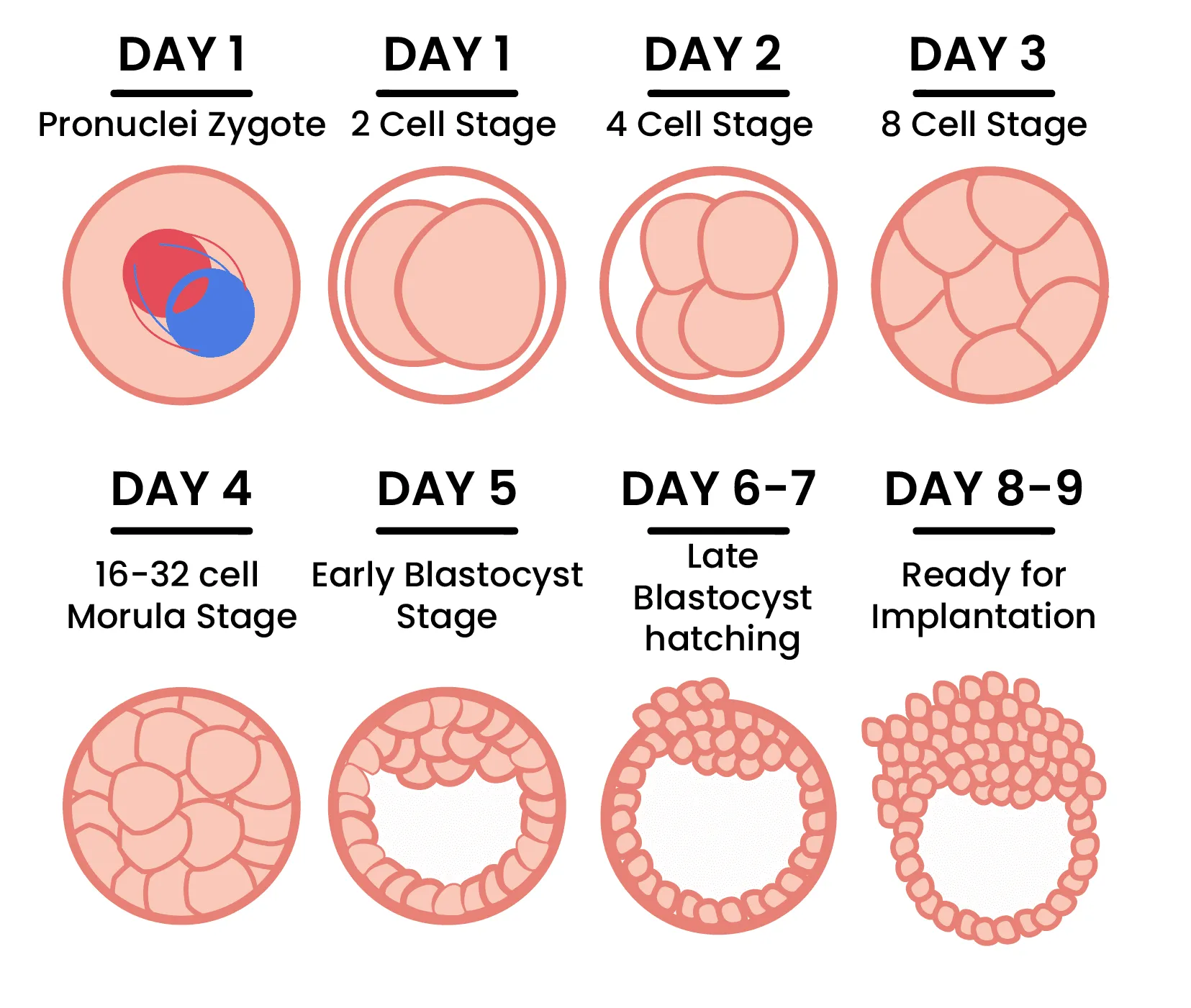
Step 4: Growing the Embryos
The embryos chill in the lab for 3-5 days, growing and developing. Scientists keep an eye on them, picking the healthiest ones for the next step. Any extras? They can be frozen for later, like putting leftovers in the freezer for another meal.
Step 5: Transferring the Embryo
Finally, one or two embryos are placed into the woman’s uterus using a thin tube called a catheter. No anesthesia needed—it’s quick and feels a bit like a Pap smear. If the embryo sticks to the uterine wall (implantation), pregnancy begins. About two weeks later, a blood test confirms if it worked.
This process usually takes 4-6 weeks per cycle, and while it’s not a guarantee, it’s a powerful tool for many. Pretty cool, right?
Why People Turn to IVF
IVF isn’t something you stumble into—it’s a choice made after facing real challenges. So, who uses it, and why? Here are some common reasons:
- Blocked Fallopian Tubes: If the tubes that carry eggs to the uterus are damaged or blocked, sperm can’t reach the egg naturally. IVF skips that step entirely.
- Low Sperm Count: When a man’s sperm isn’t strong enough to make the journey, IVF can pair it directly with an egg in the lab.
- Endometriosis: This condition messes with the reproductive system, but IVF can help bypass the chaos.
- Age-Related Infertility: As women get older, egg quality drops. IVF can use donor eggs or give older moms a better shot.
- Unexplained Infertility: Sometimes, doctors can’t pinpoint the problem. IVF steps in as a catch-all solution.
- Same-Sex Couples or Single Parents: For those who need donor eggs, sperm, or a surrogate, IVF makes parenthood possible.
Take Sarah, a 38-year-old teacher I heard about from a friend. After years of trying to conceive with no luck, she learned her fallopian tubes were scarred from an old infection. IVF was her golden ticket—after two cycles, she welcomed twins. Stories like hers show why IVF is more than a medical term; it’s a game-changer.
The Science Behind IVF: What Makes It Tick?
IVF isn’t magic—it’s science at its finest. Let’s peek under the hood at what powers this process.
Hormones Are the MVPs
Fertility drugs like FSH (follicle-stimulating hormone) and LH (luteinizing hormone) tell your ovaries to produce more eggs. Later, progesterone preps your uterus to welcome an embryo. These hormones mimic what your body does naturally, just on overdrive.
Lab Precision Matters
In the lab, conditions are perfect—temperature, light, and nutrients are all controlled to help eggs and sperm thrive. According to a 2023 study from the National Institutes of Health, embryo culture techniques have improved so much that success rates are climbing every year.
Timing Is Everything
Doctors use ultrasounds to watch your follicles (the sacs holding eggs) grow. When they hit 18-20 millimeters, it’s go-time for retrieval. Miss that window, and the eggs might not be viable.
Here’s a fun fact: Did you know the first IVF baby was born from a “natural cycle” with no fertility drugs? Today, that’s rare—stimulated cycles give better odds by producing more eggs.
Success Rates: What Are Your Chances?
IVF isn’t a sure thing, and that’s something everyone should know upfront. Success depends on a bunch of factors, like age, health, and even luck. Here’s a breakdown based on 2021 data from the CDC:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50.8% |
| 35-37 | 38.2% |
| 38-40 | 24.6% |
| Over 40 | 7.9% |
- Age: Younger women have higher success rates because their eggs are healthier.
- Embryo Quality: Fresh or frozen, the best embryos have the best shot.
- Number of Cycles: One try might not cut it—many need 2-3 cycles.
Want to test your IVF knowledge? Try this quick quiz:
Mini Quiz: What Affects IVF Success?
- Does age matter? (A) Yes (B) No
- Can frozen embryos work as well as fresh ones? (A) Yes (B) No
- Is one cycle always enough? (A) Yes (B) No
(Answers: 1-A, 2-A, 3-B)
The takeaway? IVF offers hope, but it’s not a one-size-fits-all fix. Talk to your doctor about your odds—they’ll crunch the numbers based on your unique situation.
The Emotional Rollercoaster of IVF
IVF isn’t just a physical journey; it’s an emotional one too. Picture this: You’re excited one day, nervous the next, and maybe even heartbroken if it doesn’t work. That’s normal, and you’re not alone.
The Highs
- Hearing “We got healthy embryos!” feels like winning the lottery.
- A positive pregnancy test after weeks of waiting? Pure joy.
The Lows
- Negative results sting, especially after so much effort.
- The cost—about $12,000-$17,000 per cycle—adds stress if insurance doesn’t cover it.
A 2024 survey I dug into from the American Society for Reproductive Medicine found that 70% of IVF patients felt anxious during treatment, but 85% said support from family, friends, or groups made it bearable. So, lean on your crew—whether it’s a partner, a pal, or an online community.
Tip: Join a fertility support group. Sharing stories with people who get it can lighten the load.
Risks and Realities: What to Watch For
IVF is safe, but it’s not risk-free. Knowing what could happen helps you prepare.
Common Side Effects
- Bloating or Mood Swings: Those hormone shots can make you feel off.
- Bruising: Injections leave little marks—nothing major.
Rare but Serious Risks
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can overwork your ovaries, causing pain or swelling. It hits about 1-5% of patients, per the Mayo Clinic, and usually resolves with rest.
- Multiple Births: Transferring more than one embryo ups the chance of twins or triplets, which can mean preterm delivery.
Myth-Busting Time
❌ IVF causes cancer: Studies, like one from the NIH in 2022, show no solid link between fertility drugs and ovarian cancer.
✔️ IVF babies are healthy: Research says they’re just as strong as naturally conceived kids.
Talk to your doctor about risks—they’ll tailor the plan to keep you safe.
Costs and Coverage: Breaking the Bank?
IVF isn’t cheap, but it’s not always out of reach. Here’s the scoop:
- Average Cost: $12,000-$17,000 per cycle, including meds, tests, and procedures.
- Insurance: Only 19 states in the U.S. require some infertility coverage, per Resolve.org. Check your plan!
- Options: Clinics offer payment plans, and some nonprofits give grants.
Hack: Ask your clinic about “mini IVF”—it uses fewer drugs and costs less, though success rates might dip.
I crunched some numbers: If you save $500 a month, you could fund a cycle in 2-3 years. Worth it? That’s your call.
New Twists on IVF: Beyond the Basics
IVF keeps evolving, and some lesser-known angles deserve a spotlight—stuff the top Google articles barely touch.
Natural Cycle IVF
No drugs, just your body’s one egg. It’s cheaper (around $5,000-$7,000) and gentler, but the success rate is lower—about 10-15% per cycle, says a 2023 Fertility and Sterility study. Great for women who can’t handle hormones.
Reciprocal IVF
For same-sex female couples, one partner donates the egg, and the other carries the baby. It’s a beautiful way to share parenthood, and it’s gaining traction—X posts in 2025 show it’s trending among LGBTQ+ families.
Fertility Preservation
Not ready for kids? Freeze your eggs now, use IVF later. A 2024 report from the CDC says egg freezing jumped 20% since 2020, especially for women in their 30s dodging the biological clock.
These options show IVF isn’t one-size-fits-all—it’s adapting to real lives.
IVF Around the World: A Global Perspective
IVF isn’t just an American story—it’s global, and how it’s done varies wildly.
- Japan: Super high-tech, but strict rules limit access for unmarried folks.
- India: Affordable (cycles can cost $2,000-$3,000), making it a hub for “fertility tourism.”
- Denmark: Tops the world with 10% of babies born via IVF, thanks to free treatment for residents.
A friend who traveled to Spain for IVF said the vibe was relaxed, and the cost was half of the U.S. Food for thought if you’re open to a trip!
Your IVF Journey: Tips to Make It Smoother
Ready to dive in? Here’s how to rock your IVF experience:
- Find the Right Clinic: Look at success rates on CDC.gov, but also vibe-check the staff. You want a team that feels like home.
- Prep Your Body: Eat well, sleep lots, and cut stress—think yoga or walks. A 2023 study linked better diets to higher IVF success.
- Ask Questions: How many embryos will they transfer? What’s the backup plan? Knowledge is power.
- Build a Support Squad: Tell a few close pals—they’ll cheer you on or bring ice cream when you need it.
Poll Time: What’s your top IVF prep tip?
- Healthy eating
- More sleep
- Stress relief
- Other (share below!)
The Future of IVF: What’s Next?
IVF’s not standing still. Here’s what’s cooking:
- AI in the Lab: Artificial intelligence is picking the best embryos faster, boosting success rates by 10%, per a 2024 Nature study.
- Gene Editing: CRISPR could zap genetic diseases before implantation—controversial, but on the horizon.
- Affordable Tech: Mini labs might slash costs, making IVF more accessible.
Imagine a world where IVF is as routine as a dental checkup. We’re not there yet, but science is pushing hard.
Real Stories: IVF in Action
Let’s wrap with a couple of tales—names changed, but the heart’s real.
- Mia, 34: After endometriosis crushed her dreams, Mia tried IVF. Three cycles later, she’s got a toddler and a freezer full of embryos for baby #2. “It’s exhausting, but worth every shot,” she says.
- Jake and Tom, 41 and 43: This couple used reciprocal IVF with a surrogate. Jake’s sperm, a donor egg, and Tom’s support made their son a reality. “We’re both dads in every way,” Jake grins.
These stories remind us: IVF isn’t just letters—it’s lives.
Final Thoughts: IVF Is More Than a Term
So, what does IVF stand for in medical terms? In vitro fertilization—eggs and sperm meeting in a lab to spark new life. But it’s bigger than that. It’s a chance for people to rewrite their futures, whether they’re battling infertility, chasing solo parenthood, or building a family their way. It’s messy, pricey, and emotional, but it’s also a testament to human grit and science’s wonders.
If IVF’s on your radar, dig deeper. Talk to doctors, read up, and connect with others who’ve been there. It’s not just a process—it’s a journey. And who knows? Maybe your story’s next.

